Array
(
[self] => https://cpd.partners.org/node?nid=53735
[first] => https://cpd.partners.org/node?nid=53735&page=0
[last] => https://cpd.partners.org/node?nid=53735&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 Credits™
Mass General Brigham designates this live activity for a maximum of 22.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 22.5 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
Physician Assistants
Mass General Brigham has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 22.5 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation.

MOC COMPLETION CRITERIA
Participant completion for MOC points will be reported to the boards at the conclusion of the course.
Please have your ABIM ID available when completing the evaluation at the end of the course.
Instructions: Medical Knowledge MOC points in the American Board of Internal Medicine's (ABIM) Maintenance of Certification (MOC) Program
Upon successful completion of this activity, if you wish to receive MOC Part 2 points you will need to enter your ABIM ID number in the post-course evaluation. The Mass General Brigham Office of Continuing Professional Development will verify completion of your activity and report to the ABIM. Diplomates must check their ABIM Portfolio for confirmation of your MOC Part 2 points.
MOC Recognition Statement
Successful completion of this CME activity, which includes participation in the activity, with individual assessments of the participant and feedback to the participant, enables the participant to earn 22.5 MOC points in the American Board of Internal Medicine (ABIM) Maintenance of Certification (MOC) program. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/197
[id] => 197
[resource] => taxonomy_term
[uuid] => 621a8034-627c-4c33-b273-260b2d83768c
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1674664200
[value2] => 1714190340
[duration] => 39526140
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1697025600
[value2] => 1697227200
[duration] => 201600
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/238
[id] => 238
[resource] => taxonomy_term
[uuid] => fd81c17a-d19b-46b8-ad6b-2c5aee9ce9be
)
[1] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/7
[id] => 7
[resource] => taxonomy_term
[uuid] => 2a38b69f-4c76-44b0-bde5-67e901205c53
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/37183
[id] => 37183
[resource] => file
[uuid] => 7f2fe396-197e-4d9c-a3a5-83a0ad45f376
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 35607
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Fairmont Copley Hotel
[street] => 138 St. James Ave
[additional] =>
[city] => Boston
[province] => MA
[postal_code] => 02116
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => Live Stream or In-Person options
Fairmont Copley Hotel, Boston, MA
OCTOBER 11-13, 2023


| Registration Type | Early Bird Rate (Before September 1, 2023) | Standard Rate (After September 1, 2023) |
|---|---|---|
| Physicians | $795.00 | $895.00 |
| Allied Health Care Professionals | $695.00 | $795.00 |
| Residents/Fellows | $600.00 | $600.00 |
This course provides a comprehensive review of state-of-the-art practices to diagnose and treat patients with cardiovascular conditions. Led by the leading clinical faculty of Harvard Medical School and the Massachusetts General Hospital (MGH) Corrigan Minehan Heart Center, Update in Clinical Cardiology ensures attendees are current with recent advances in clinical cardiology and the best ways to incorporate them into daily practice to optimize patient outcomes.
The 2023 program offers you the opportunity to learn:
- Important medical and procedural advances for the management of common clinical problems such as coronary artery disease and heart failure (including heart failure with preserved ejection fraction)
- The latest transcatheter options
- Best practices to treat patients with severe valvular disease
- Important techniques for managing heart disease in pregnancy
- The new paradigms for care of specialized populations, such as adults with congenital heart disease, cardiac patients with cancer, and athletic individuals
- The latest concepts of diagnosis, decision-making, pharmacology, and therapy in the areas of ischemic heart disease, cardiac arrhythmias, and congestive heart failure
Course Directors
Rory Weiner, MD
Associate Professor of Medicine, Harvard Medical School;
Cardiologist specializing in Echocardiography and Cardiovascular Performance, Massachusetts General Hospital
Emily Lau, MD, MPH 
Instructor in Medicine, Harvard Medical School;
Director, Hormones & Cardiovascular Disease Clinic, Massachusetts General Hospital
Nurse Planner
Susan McDermott MSN ANP-BC
Director of Advance Practice Providers Cardiology Division,
Massachusetts General Hospital
Keynote Speaker
Patrick O'Gara, MD 
Professor of Medicine, Harvard Medical School;
Director of Strategic Planning for the Cardiovascular Division, Brigham & Women's Hospital
Faculty
Erin Coglianese, MD
Assistant Professor of Medicine, Harvard Medical School;
Medical Director, Mechanical Cardiac Support Program, Massachusetts General Hospital
Douglas E. Drachman, MD
Assistant Professor of Medicine, Harvard Medical School;
Director of Education and Interventional Cardiology Fellowship Program, Massachusetts General Hospital
David Dudzinksi, MD
Assistant Professor of Medicine, Harvard Medical School;
Director of Cardiac Intensive Care Unit, Massachusetts General Hospital
Akl Fahed, MD, MPH
Instructor in Medicine, Harvard Medical School;
Interventional Cardiologist, Massachusetts General Hospital
J. Sawalla Guseh, MD
Instructor of Medicine, Harvard Medical School;
Director of Cardiovascular Performance Fellowship Program, Massachusetts General Hospital
Kevin Heist, MD, PhD
Associate Professor of Medicine, Harvard Medical School;
Cardiac Electrophysiologist, Massachusetts General Hospital
Eric Isselbacher, MD
Associate Professor of Medicine, Harvard Medical School;
Co-Director, Thoracic Aortic Center, Massachusetts General Hospital
Farouc Jaffer, MD, PhD
Associate Professor of Medicine, Harvard Medical School;
Director, Coronary Intervention; Director, MGH CTO Percutaneous Coronary Intervention Program, Massachusetts General Hospital
James Januzzi, MD
Hutter Family Professor of Medicine in the Field of Cardiology, Harvard Medical School;
Director, Dennis and Marilyn Barry Fellowship in Cardiology Research, Massachusetts General Hospital
Christopher Learn, MD
Instructor in Medicine, Harvard Medical School;
Cardiologist, Adult Congenital Heart Disease Specialist, Massachusetts General Hospital
Gregory Lewis, MD
Associate Professor of Medicine, Harvard Medical School;
Medical Director, Cardiac Transplantation Program, Director, Cardiopulmonary Exercise Testing Laboratory, Massachusetts General Hospital
Moussa Mansour, MD
Associate Professor in Medicine, Harvard Medical School;
Director, Atrial Fibrillation Program, Massachusetts General Hospital
Theofanie Mela, MD
Associate Professor of Medicine, Harvard Medical School;
Director, Lead Management Program, Cardiac Electrophysiologist, Massachusetts General Hospital
Pradeep Natarajan, MD
Associate Professor of Medicine, Harvard Medical School;
Director of Preventive Cardiology, Massachusetts General Hospital
Tomas Neilan, MD, MPH
Associate Professor of Medicine, Harvard Medical School;
Director, Cardio-Oncology Program, Massachusetts General Hospital
Michelle O'Donoghue, MD, MPH
Associate Professor of Medicine, Harvard Medical School;
Cardiologist, Brigham and Women's Hospital
Jonathan Passeri, MD
Assistant Professor of Medicine, Harvard Medical School;
Co-Director of Heart Valve Program & Director of Interventional Echocardiography, Massachusetts General Hospital
Nilay Patel, MD
Instructor in Medicine, Harvard Medical School;
Interventional Cardiologist, Massachusetts General Hospital
Marc Sabatine, MD, MPH
Professor of Medicine, Harvard Medical School;
Cardiologist, Massachusetts General Hospital
Rahul Sakhuja, MD, MPP
Instructor in Medicine, Harvard Medical School;
Interventional Cardiologist, Massachusetts General Hospital
Nandita Scott, MD
Assistant Professor of Medicine, Harvard Medical School;
Co-Director Corrigan Women's Heart Health Program, Director, Cardiovascular Medicine Section, Massachusetts General Hospital
Jagmeet Singh, MD, PhD
Professor of Medicine, Harvard Medical School;
Founding Director, Resynchronization and Advanced Cardiac Therapeutics Program, Massachusetts General Hospital
Albree Tower-Rader, MD
Instructor in Medicine, Harvard Medical School;
Cardiologist, Cardiac Radiologist, Massachusetts General Hospital
Ido Weinberg, MD
Associate Professor of Medicine, Harvard Medical School;
Director, Vascular Medicine Fellowship, Massachusetts General Hospital
Daniel Zlotoff, MD, PhD
Instructor in Medicine, Harvard Medical School;
Heart Failure & Transplant Cardiologist, Massachusetts General Hospital
Accommodations
FAIRMONT COPLEY PLAZA
138 ST. JAMES AVENUE
BOSTON, MA 02116
PHONE: 617-267-5300
MUST SPECIFY ATTENDING THE UPDATE IN CLINICAL CARDIOLOGY COURSE TO OBTAIN THESE RATES WHEN BOOKING
| Single Rate | Double Rate | |
| Moderate & Fairmont Room (One Queen Bed) | $399.00 | $399.00 |
| Deluxe Room (One King Bed or Two Double Beds) | $439.00 | $439.00 |
Room assignment is based on guest preferences and availability at the time of request.
[format] => full_html ) [field_hotel_link] => Array ( ) [field_hotel_photo] => Array ( ) [field_hotel_travel] => Array ( ) [field_learning_objectives] => Array ( [value] =>Upon completion of this activity, participants will be able to:
- Apply newly acquired knowledge of cardiovascular disease in the care of cardiac patients.
- Incorporate the principles of proper evaluation for cardiovascular disease into practice.
- Determine the goals to be achieved in the care of cardiovascular patients and implement tools to achieve these goals.
- Use diagnostic and therapeutic tools to treat patients with cardiovascular disease appropriately.
- Demonstrate active information sharing amongst participants and speakers so that the entire healthcare team in attendance obtains information that can be utilized to improve clinical practice and patient care.
Wednesday, October 11, 2023 | 7:50am - 5:00pm
Morning Moderator: Rory B. Weiner, MD
Afternoon Moderator: Emily S. Lau, MD, MPH
| 7:50am | Introduction | Rory B. Weiner, MD |
| 8:00 | What's New in Cardiac Markers | James L. Januzzi, MD |
8:40 | Q&A Session | James L. Januzzi, MD |
8:50 | The New Role of the Cardiologist in Diabetes Management | James L. Januzzi, MD |
9:30 | Q&A Session | James L. Januzzi, MD |
9:40 | MORNING BREAK |
9:55 | Aortic Stenosis: Timing of Intervention and Choosing Between Surgery and Percutaneous Therapy | Nilay Patel, MD |
10:35 | Q&A Session | Nilay Patel, MD |
10:45 | Transcatheter procedures in the Cath Lab: Imaging and Intervention | Jonathan Passeri, MD |
11:25 | Q&A Session | Jonathan Passeri, MD |
11:35 | Inaugural Adolph M. Hutter, Jr., MD Lecture | Patrick T. O’Gara, MD |
12:15pm | Q&A Session | Patrick T. O’Gara, MD |
12:25 | LUNCH BREAK |
1:20 | Advances in Medical Treatment of Systolic Heart Failure | Daniel Zlotoff, MD, PhD |
| 2:00 | Q&A Session | Daniel Zlotoff, MD, PhD |
2:10 | Advanced Heart Failure: Acute and Chronic Therapy | Erin Coglianese, MD |
2:50 | Q&A Session | Erin Coglianese, MD |
3:00 | AFTERNOON BREAK |
3:15 | Heart Failure with Preserved Ejection Fraction (HFpEF) | Gregory D. Lewis, MD |
3:55 | Q&A Session | Gregory D. Lewis, MD |
4:05 | Cardiac Critical Care | David Dudzinski, JD, MD |
4:45 | Q&A Session | David Dudzinski, JD, MD |
| 5:00pm | Adjourn |
Thursday, October 12, 2023 | 7:55am - 5:00pm
Morning Moderator: Rory B. Weiner, MD
Afternoon Moderator: Emily S. Lau, MD, MPH
| 7:55am | Introduction | Rory B. Weiner, MD |
| 8:00 | Incorporating Advances in Electrical Therapy in Heart Failure for Improved Patient Outcomes | Jagmeet P. Singh, MD, PhD |
8:40 | Q&A Session | Jagmeet P. Singh, MD, PhD |
8:50 | Atrial Fibrillation: Recent Advances in Pharmacologic and Nonpharmacologic Therapy | Moussa Mansour, MD |
9:30 | Q&A Session | Moussa Mansour, MD |
9:40 | MORNING BREAK |
9:55 | The Newest Approaches to Stroke Prevention in Atrial Fibrillation | Kevin Heist, MD, PhD |
10:35 | Q&A Session | Kevin Heist, MD, PhD |
10:45 | Supraventricular Tachycardia (SVT) in 2023 | Theofanie Mela, MD |
11:25 | Q&A Session | Theofanie Mela, MD |
11:35 | Thoracic Aortic Disease: Updates from New Practice Guidelines | Eric M. Isselbacher, MD |
12:15pm | Q&A Session | Eric M. Isselbacher, MD |
12:25 | LUNCH BREAK |
1:20 | Dyslipidemia: Latest Concepts | Pradeep Natarajan, MD |
| 2:00 | Q&A Session | Pradeep Natarajan, MD |
2:10 | Acute Coronary Syndromes- STEMI and NSTEMI: The New Data and Clinical Implications | Marc Sabatine, MD, MPH |
2:50 | Q&A Session | Marc Sabatine, MD, MPH |
3:00 | AFTERNOON BREAK |
3:15 | Dual Antiplatelet Therapy in Cardiovascular Disease | Michelle L. O’Donoghue, MD |
3:55 | Q&A Session | Michelle L. O’Donoghue, MD |
4:05 | Coronary Disease: Medicate/Dilate/Operate | Rahul Sakhuja, MD |
4:45 | Q&A Session | Rahul Sakhuja, MD |
| 5:00pm | Adjourn |
Friday, October 13, 2023 | 7:55am - 5:00pm
Morning Moderator: Rory B. Weiner, MD
Afternoon Moderator: Emily S. Lau, MD, MPH
| 7:55am | Introduction | Rory B. Weiner, MD |
| 8:00 | Peripheral Arterial Disease in 2023 | Douglas E. Drachman, MD |
8:40 | Q&A Session | Douglas E. Drachman, MD |
8:50 | Pulmonary Embolism | Ido Weinberg, MD |
9:30 | Q&A Session | Ido Weinberg, MD |
9:40 | MORNING BREAK |
9:55 | State-of-the-Art Approaches to Cardio-Oncology | Tom Neilan, MD |
10:35 | Q&A Session | Tom Neilan, MD |
10:45 | Specialized Procedures in the Cardiac Cath Lab | Akl Fahed, MD & Farouc Jaffer, MD, PhD |
11:25 | Q&A Session | Akl Fahed, MD & Farouc Jaffer, MD, PhD |
11:35 | Update in Cardiovascular Disease and Pregnancy | Nandita Scott, MD |
12:15pm | Q&A Session | Nandita Scott, MD |
12:25 | LUNCH BREAK |
1:20 | INOCA: Ischemia with Non-Obstructive Coronary Arteries | Emily S. Lau, MD, MPH |
| 2:00 | Q&A Session | Emily S. Lau, MD, MPH |
2:10 | Cardiomyopathies with LV Hypertrophy | Albree Tower-Rader, MD |
2:50 | Q&A Session | Albree Tower-Rader, MD |
3:00 | AFTERNOON BREAK |
3:15 | Evaluation and Treatment of Adult Congenital Heart Disease | Christopher Learn, MD |
3:55 | Q&A Session | Christopher Learn, MD |
4:05 | Sports Cardiology | J. Sawalla Guseh, MD |
4:45 | Q&A Session | J. Sawalla Guseh, MD |
| 4:55 | Closing Remarks | Rory B. Weiner, MD |
| 5:00pm | Adjourn |
Accommodations
FAIRMONT COPLEY PLAZA
138 ST. JAMES AVENUE
BOSTON, MA 02116
PHONE: 617-267-5300
MUST SPECIFY ATTENDING THE UPDATE IN CLINICAL CARDIOLOGY COURSE TO OBTAIN THESE RATES WHEN BOOKING
| Single Rate | Double Rate | |
| Moderate & Fairmont Room (One Queen Bed) | $399.00 | $399.00 |
| Deluxe Room (One King Bed or Two Double Beds) | $439.00 | $439.00 |
Room assignment is based on guest preferences and availability at the time of request.
| Registration Type | Early Bird Rate (Before September 1, 2023) | Standard Rate (After September 1, 2023) |
|---|---|---|
| Physicians | $795.00 | $895.00 |
| Allied Health Care Professionals | $695.00 | $795.00 |
| Residents/Fellows | $600.00 | $600.00 |
Cancellation Policy:
Registrations cancelled on or before September 28, 2023 will be refunded, less a $100 administrative fee. Registrations cancelled after September 28, 2023 will not be refunded.
Contact partnerscpd@partners.org if you require assistance in cancelling your online registration.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for Physicians, Nurses, Physician Assistants in the following specialties Cardiology, Critical Care, Emergency Medicine, General Practice, Geriatric Medicine, Hematology/Oncology, Internal Medicine, Interventional Cardiology, Obstetrics/Gynecology, Peripheral Vascular Disease, Primary Care, Pulmonary Disease, and Sports Medicine.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/2374 [id] => 2374 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital - Corrigan Minehan Heart Center and
Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=69481
[first] => https://cpd.partners.org/node?nid=69481&page=0
[last] => https://cpd.partners.org/node?nid=69481&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Mass General Brigham designates this live activity for a maximum of 7.50 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/236
[id] => 236
[resource] => taxonomy_term
[uuid] => eb0ec44a-4c85-40f2-9c3b-b8a19a3d44a9
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1705496400
[value2] => 1718337540
[duration] => 12841140
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1715341500
[value2] => 1715374800
[duration] => 33300
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/61722
[id] => 61722
[resource] => file
[uuid] => b7b3cf2f-6731-40d7-8082-70dd0681d399
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => THIS IS A VIRTUAL COURSE
Midlife Women’s Health 2024 provides a multi-disciplinary approach to the care of menopausal women. Advances in research, technology, and pharmacology increase options available for midlife women, but this rapidly changing knowledge-base presents a challenge for clinicians. Care for women at this stage of life is optimized by education on a range of medical concerns provided by experts from a wide variety of medical specialties. Given demographic changes in the US population, midlife women are becoming an increasingly important group served by health care professionals, with needs that cross many areas of medical expertise.
In this educational activity, a multidisciplinary group of experts from Massachusetts General Hospital will present on the evaluation and management of gynecologic cancers, vascular disease, parathyroid disease and thyroid nodules, vulvovaginal disorders, lung cancer, cardiovascular health, attention deficit hyperactivity disorder, sexuality after cancer, and menopausal hormone therapy to assist clinicians in caring for their midlife patients.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Jan L. Shifren, MD - Course Director
Jan L. Shifren, MD is a reproductive endocrinologist at the Massachusetts General Hospital and Director of the MGH Midlife Women’s Health Center. She is the Vincent Trustees Professor of Obstetrics, Gynecology and Reproductive Biology at Harvard Medical School. Dr. Shifren focuses her research on menopause, including the effects of estrogens, androgens and alternative therapies on menopausal symptoms and sexual function. She is a past President of the Menopause Society.
Allison Baker, MD
Allison Baker, MD is a psychiatrist with the Perinatal and Reproductive Psychiatry Clinical Research Program at the Massachusetts General Hospital and an Instructor in Psychiatry at Harvard Medical School. Her current research focuses on the course and treatment of ADHD in women during pregnancy and postpartum.
Don Dizon, MD
Don Dizon, MD is the Director of the Pelvic malignancies Program at Lifespan Cancer Institute, Head of Community Outreach & Engagement at Legorreta Cancer Center, and the Director of Medical Oncology at Rhode Island Hospital. Nationally, he is the Vice Chair for Diversity, Equity, Inclusion, and Professional Integrity at SWOG Cancer Research Network. He also is a founding member of the Collaboration for Outcomes using Social Media in Oncology. His research foci include novel treatment of ovarian, uterine, and cervical cancers; communication; survivorship after cancer especially in sexuality; professional social media use; and advocacy on behalf of the sexual and gender minoritized communities.
Anahita Dua, MD, MS, MBA
Anahita Dua, MD, MS, MBA is a vascular surgeon at the Massachusetts General Hospital and an Associate Professor of Surgery at Harvard Medical School. At MGH, she is the director of the Vascular Lab, co-director of the Peripheral Artery Disease Center and Limb Evaluation and Amputation Program, associate director of the Wound Care Center, director of the Lymphedema Center, associate director of the Vascular Surgery Clerkship, and director of clinical research for the division of vascular surgery.
Rajshri Gartland, MD, MPH
Rajshri Gartland, MD, MPH is an endocrine surgeon and surgical oncologist at the Massachusetts General Hospital with expertise in the surgical treatment of benign and malignant thyroid, parathyroid, and adrenal diseases. Dr. Gartland's clinical and research interests focus on the practice and advancement of endocrine surgery, particularly through innovative and minimally-invasive techniques. She co-founded and leads the Thyroid Radiofrequency Ablation Program at MGH and serves as Surgical Director of the NWH Thyroid Biopsy Clinic and Assistant Chief Quality Officer at MGH.
Allison Gockley, MD
Allison Gockley, MD is a gynecologic oncologist in the Department of Obstetrics and Gynecology at the Massachusetts General Hospital. Dr. Gockley’s research interests include the surgical treatment of gynecologic cancers, gestational trophoblastic neoplasia, advanced endometrial cancer and onco-fertility.
Linda Kelly, DNP, ANP-BC
Linda Kelly, DNP, ANP-BC is an advanced practice provider at the Massachusetts General Hospital. She is the Nursing Director of the Midlife Women's Health Center in the Department of Obstetrics and Gynecology at the Massachusetts General Hospital.
Deborah Kwolek, MD
Deborah Kwolek, MD is a primary care physician at the Massachusetts General Hospital and the founding lead of the Women’s Health and Sex and Gender Medicine Program at the MGH and Harvard Medical School. Dr Kwolek is co-editor of the textbook, Sex- and Gender-Based Women’s Health: A Practical Guide for Primary Care. She is Chair of the Society of General Internal Medicine’s Women and Medicine Commission and serves as Co-Chair of the American Medical Women’s Association’s Sex and Gender Health Collaborative’s mentoring committee. Dr. Kwolek directs the HMS Primary Care Internal Medicine Course and the Women's Health Resident Rotation at MGH.
Varvara Mazina, MD
Varvara Mazina, MD is a gynecologic oncologist in the Department of Obstetrics and Gynecology at the Massachusetts General Hospital. Dr. Mazina’s research interests include multidisciplinary and translational collaboration for management of gynecologic malignancies, surgical innovation and education, and improvement of quality of life of cancer patients and survivors.
Alisa Pascale, DNP, WHNP-BC
Alisa Pascale, DNP, WHNP-BC is a women's health nurse practitioner in the Department of Obstetrics and Gynecology at the Massachusetts General Hospital. Her clinical interests include routine gynecologic care across the lifespan, contraceptive management, perimenopausal issues and LGBTQ health. She has clinical expertise in vulvar and vaginal disorders, including chronic vaginitis, and vulvar skin disorders such as lichen sclerosis. Dr. Pascale is a clinical instructor in the Women's Health program at the MGH Institute of Health Professions.
Isaac Schiff, MD
Isaac Schiff, MD is the Chief, Department of Obstetrics and Gynecology, Emeritus, at the Massachusetts General Hospital and the Joe Vincent Meigs Distinguished Professor of Gynecology at Harvard Medical School. He is Co-Director of the MGH Midlife Women’s Health Center. Dr. Schiff is an internationally known expert in menopause, a founding member of the Menopause Society, and the Editor-in-Chief of the journal, Menopause.
Lecia Sequist, MD, MPH
Lecia Sequist, MD, MPH is a medical oncologist in the Center for Thoracic Cancers at the Massachusetts General Hospital and Program Director, Cancer Early Detection and Diagnostics Clinic. She holds the Mary B Saltonstall Endowed Chair in Oncology at MGH and is the Landry Family Professor of Medicine at Harvard Medical School. Dr. Sequist's research focuses on studying novel targets and targeted agents for lung cancer treatment and in detecting and studying the significance of tumor cells circulating in the bloodstream.
Ahmed Tawakol, MD
Ahmed Tawakol, MD is a cardiologist at the Massachusetts General Hospital. He is Co-Director of the Cardiac MR PET CT Program. Dr. Tawakol's research focuses on developing novel diagnostic approaches and treatment strategies for atherosclerosis. He leads several multi-center trials to evaluate interventions targeting plaque inflammation and is evaluating the potential clinical role of vascular PET imaging for improving the identification of patients at highest risk for atherothrombotic events.
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Identify signs and symptoms of gynecologic cancers at midlife to optimize outcomes.
- Employ a greater understanding of vascular disease in aging women to reduce disease burden.
- Evaluate parathyroid disease and thyroid nodules in aging women.
- Assess midlife women for vulvovaginal disorders and guide the use of available treatment options.
- Recognize the link between stress, inflammation, and cardiovascular disease in women to improve health.
- Assess midlife women for attention deficit hyperactivity disorder and utilize effective therapies.
- Formulate a strategy to identify women at increased risk of lung cancer to optimize care.
- Integrate behavioral and pharmacologic strategies to improve sexual function for cancer survivors.
- Evaluate symptomatic midlife women for menopausal hormone therapy, incorporating an individualized assessment of risks and benefits.
[format] => full_html
)
[field_program] => Array
(
[value] => 7:45 AM | Welcome & Introductory Remarks |
8:00 | Gynecologic Cancers: Update for 2024 |
8:45 | Vascular Disease: Evaluation and Treatment in Older Women |
9:30 | Parathyroid Disease and Thyroid Nodules: Diagnosis and Management |
10:15 | Break |
10:30 | Vulvovaginal Disorders at Midlife: Beyond the Genitourinary Syndrome of Menopause |
11:15 | Stress, Inflammation & Cardiovascular Disease: Understanding the Link in Aging Women |
12:00 PM | Lunch Break |
1:00 | Beyond Adolescence - Impact of Attention Deficit Hyperactivity Disorder in Midlife Women |
1:45 | Lung Cancer in Women: Optimizing Identification & Treatment |
2:30 | Sexuality after Cancer |
| 3:15 | Break |
3:30 | Menopausal Hormone Therapy - Risks, Benefits & Alternatives |
4:15 | Everything You Wanted to Know About Menopause, but Were Afraid to Ask |
5:00 PM | Adjournment |
[format] => full_html ) [field_registration_instructions] => Array ( [value] =>
BEFORE MARCH 29, 2024
| Registration Type | Tuition Fee |
|---|---|
| Physician | $270 |
| Other Health Care Professionals & Physicians-in-Training | $125 |
AFTER MARCH 29, 2024
| Registration Type | Tuition Fee |
|---|---|
| Physician | $295 |
| Other Health Care Professionals & Physicians-in-Training | $150 |
Cancellation Policy:
Registrations cancelled on or before March 29, 2024 will be refunded, less a $35 administrative fee. Registrations cancelled after March 29, 2024 will not be refunded.
Contact partnerscpd@partners.org if you require assistance in cancelling your online registration.
Please contact our Course Coordinator at MGHMidlifeCenter@mgh.harvard.edu prior to the event to assist you with any special needs.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This educational activity is intended for physicians and advance practice nurses in primary care, gynecology, general surgery, internal medicine, endocrinology, psychiatry, gynecological oncology, cardiology, and preventive medicine who provide care to midlife women. Physicians and advance practice nurses in-training also are encouraged to attend.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3119 [id] => 3119 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital - Department of OB/GYN & Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=81317
[first] => https://cpd.partners.org/node?nid=81317&page=0
[last] => https://cpd.partners.org/node?nid=81317&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => 
In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditTM
Mass General Brigham designates this enduring activity for a maximum of 15 AMA PRA Category 1 CreditTM (per session). Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 15ANCC contact hour (per session). Nurses should only claim credit commensurate with the extent of their participation in the activity.
Social Work
As a Jointly Accredited Organization, Mass General Brigham is approved to offer social work continuing education by the Association of Social Work Boards (ASWB) Approved Continuing Education (ACE) program. Organizations, not individual courses, are approved under this program. State and provincial regulatory boards have the final authority to determine whether an individual course may be accepted for continuing education credit. Mass General Brigham maintains responsibility for this course. Social workers completing this course receive 1 continuing education credit (per session).
Lifelong Learning Maintenance of Certification (MOC) Program
American Board of Internal Medicine's (ABIM)
MOC COMPLETION CRITERIA
Participant completion for MOC points will be reported to the boards when credit is awarded for the session.
MOC points can only be awarded if you attended the entire session.
Lifelong Learning MOC points in the American Board of Internal Medicine's (ABIM) Maintenance of Certification (MOC) Program
Upon successful completion of this activity, if you wish to receive MOC Part 2 points you will need to enter your ABIM ID number and birthday (month/day) in your profile. The Mass General Brigham Office of Continuing Professional Development will verify completion of the activity and report to the ABIM. . Diplomates are responsible for checking their ABIM Portfolio for confirmation of MOC Part 2 points.
MOC RECOGNITION STATEMENT
Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to 15 MOC point (per session) in the American Board of Internal Medicine’s (ABIM) Maintenance of Certification (MOC) program. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1746532800
[value2] => 1782878340
[duration] => 36345540
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/86706
[id] => 86706
[resource] => file
[uuid] => 0a63bde8-8739-4265-bea0-d988d122c98f
)
)
[field_course_intro] => Array
(
)
[field_course_live] =>
[field_course_location] => Array
(
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => This activity provides on-demand lectures from the MGH Palliative Care and Geriatric Medicine Grand Rounds series, administered by the Harvard Medical School Center for Palliative Care.
The MGH Palliative Care and Geriatric Medicine Grand Rounds convene leading speakers from inside the Harvard Medical School network and from across the country to speak to the highest priority issues in caring for patients and families at the end of life.
Presenters for MGH Palliative Care and Geriatric Medicine Grand Rounds are invited through a rigorous review process. We host sessions that span a wide range of topics of interest to palliative care and geriatric medicine clinicians to inform effective, patient-centered practice. MGH Palliative Care and Geriatric Medicine Grand Rounds offers a distinctive opportunity to learn about leading research and to stay current with best practices.
The mission of the Harvard Medical School Center for Palliative Care is to foster an interdisciplinary community of clinicians, educators, and researchers to promote and disseminate compassionate, evidence-based care for all people living with serious illness and their families.
We encourage teams to enroll in the course and Group Discounts are available -- please contact the HMS Center for Palliative Care at pallcare@partners.org
Course Director: Khadidjatou Kane, MD
For questions regarding the registration process, please contact Mass General Brigham Office of Continuing Professional Development at mgbcpd@mgb.org.
You may print individual certificates throughout the year; your cumulative list of sessions attended is accessible on your transcript.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Course Director
Khadidjatou Kane, MD
Massachusetts General Hospital
DISCLOSURE SUMMARY OF RELEVANT FINANCIAL RELATIONSHIPS
MITIGATION STRATEGIES
Mass General Brigham has implemented a process to mitigate relevant financial relationships for this continuing education (CE) activity to help ensure content objectivity, independence, fair balance and ensure that the content is aligned with the interest of the public.
The following planners reported no relevant financial relationship with an ineligible company:
Khadidjatou Kane, MD
Terrance P. Murphy, MD
Simone Rinaldi, MSN, ANP-BC, ACHPN
Todd Rinehart, LICSW, APHSW-C
The following speakers reported no relevant financial relationship with an ineligible company:
Michelle Diop, MD
Stephanie Kiser, MD, MPH
Katie Jones Fitzgerald, PhD, ACHPN, CARN-AP
Corey Fehnel, MD
David Hao, MD
Abby Rosenberg, MD
Irene Yeh, MD, MPH
Charmaine Lastimoso
Sarah Byrne-Martelli, DMin, BCC
Dorreen Danesh, MD
Manuel Fanarjian, MD
Blair Robinson, MD
Jameson Cooper, SLP
Courtney Munro, SLP
Peter Rabins, MD, MPH
Anna Gosline
Kimberly Angelia Curseen, MD
The following speakers reported a relevant financial relationship with an ineligible company:
Sharl Azar, MD
Grant Support/Consulting, Vertex Pharmaceuticals
Grant Support, GBT/Pfizer
Lisa LaRowe, PhD
Research Funding, Google/YouTube
Joseph Greer, PhD
Research Support: Blue Note Therapeutics
Consultant: BeiGene
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Demonstrate how interprofessional learning can lead to better team integration, sustainability, and collaboration in Palliative Care and Geriatric Medicine.
- Describe pain management practices, including for cancer patients, aging patients, and patients with substance use disorder.
- Describe whole person assessment and care, including supportive care for seriously ill patients.
- Describe palliative and geriatric medicine care for patients with certain conditions and/or in particular settings.
- Describe innovative research and practices in palliative care
[format] => full_html
)
[field_program] => Array
(
[value] => MGH Palliative Care and Geriatric Medicine Grand Rounds and Harvard Medical School Center for Palliative Care: Video Sessions for First Course
| Title | Presenter(s) |
|
| “Bridging the Gap: Palliative Care for Adults Living with Sickle Cell Disease” | Sharl Azar, MD is a Hematologist at the Massachusetts General Hospital and Harvard Medical School and the Medical Director of the Comprehensive Sickle Center Disease Treatment Center. |
|
|
| Michelle Diop, MD, ScM is an Attending Physician at Massachusetts General Hospital |
|
|
| Stephanie Kiser, MD, MPH is an Attending Physician in the Department of Internal Medicine, Division of Palliative Care and Geriatric Medicine and the Clinical Director for Palliative Care at Massachusetts General Hospital and Instructor in Medicine, Harvard Medical School. |
|
|
|
|
|
| “Chronic Pain in Aging and Serious Illness: Clinical Practice Pearls” | Katie Fitzgerald Jones, PhD, ACHPN, CARN-AP is a Palliative and Addiction Nurse Practitioner, Section of Palliative Care, VA Boston Healthcare System and Instructor, Department of Medicine, Harvard Medical School. |
|
|
| Lisa LaRowe, PhD is a Research Faculty Member at the Mongan Institute Center for Aging and Serious Illness at the Mass General Research Institute and Instructor of Medicine at Harvard Medical School. |
|
|
|
|
|
| “Honoring Wishes on an Unclear Path: Aging and Palliative Care in the ICU” | Corey Fehnel, MD, MPH is the Division Chief, Neurocritical Care and Hospital Neurology at Beth Israel Deaconess Medical Center and Assistant Professor of Neurology, Harvard Medical School |
|
|
|
|
|
| “What About a Nerve Block? Interventions for Cancer-Related Pain | David Hao, MD is a double board-certified anesthesiologist and chronic pain physician at Massachusetts General Hospital, where he also serves as the Director of the MGH Cancer Pain Program |
|
|
|
|
|
| “The Science and Art of Resilience: Lessons Learned from Patients, Families, and Communities” | Abby R. Rosenberg, MD, MS, MA joined the team at Boston Children's Hospital as the Director of Palliative Care in 2023. She is also the Chief of Pediatric Palliative Care at the Dana-Farber Cancer Institute. |
|
|
|
|
|
| “Enhancing Coping in Patients with Advanced Cancer | Joseph Greer, PhD is the Co-Director of the Cancer Outcomes Research & Education Program at the Massachusetts General Hospital Cancer Center. He is also an Associate Professor of Psychology at Harvard Medical School. |
|
|
|
|
|
| “Moving Beyond ‘Tell Me More’: Level Up Your Approach to Cross-Cultural Interactions | Irene M. Yeh, MD, MPH, FAAHPM is a Senior Physician in the Department of Supportive Oncology at Dana-Farber Cancer Institute and an Instructor in Medicine at Harvard Medical School. |
|
|
|
|
|
| “Naming the SHAME: Talking about Substance Use Disorder and Complex Pain in Palliative Care” | Charmaine Lastimoso, MSN, MPH, NP-C, CARN-AP is a Palliative Care Nurse Practitioner with the Department of Supportive Oncology at the Dana-Farber Cancer Institute |
|
|
|
|
|
| “Spiritual Care for Generalists and Specialists: Integrating Research and Practice” | Sarah Byrne-Martelli, DMin, MDiv, BCC-PCHAC is a Palliative Care Researcher, at Massachusetts General Hospital Center for Aging and Serious Illness and Assistant Professor of Spiritual Care, St. Vladimir’s Orthodox Theological Seminary |
|
|
|
|
|
| “Shackled at the End of Life: Palliative Care in the Context of a Growing Incarcerated Geriatric Population” | Dorreen Danesh, MD is a PACE Physician at San Ysidro Health. |
|
|
|
|
|
| “Artificial Intelligence in Serious Illness Care” | Manuel Fanarjian, MD is a palliative care physician and clinical informaticist at Dana-Farber Cancer Institute, as well as an Instructor in Medicine at Harvard Medical School. |
|
|
|
|
|
| “Strengthening Palliative Care Partnership with Speech Language Pathology: Reframing the narrative for seriously ill patients with dysphagia and communication vulnerabilities” | Blair Robinson, MD, MPH at Massachusetts General Hospital and Instructor in Medicine
|
|
|
| Jameson Cooper, MS, CCC-SLP is a Research Speech Language Pathologist at the MGH Center for Laryngeal Surgery and Voice Rehabilitation |
|
|
| Courtney Munro is a Speech Language Pathologist at Massachusetts General Hospital |
|
|
|
|
|
| “Palliative Care for People with Dementia” | Peter Rabins, MD was the founding director of the division of geriatric psychiatry at the Johns Hopkins School of Medicine in Baltimore, MD and the first holder of the Richman Family Chair of Alzheimer’s disease and Related Disorders. |
|
|
|
|
|
| “What We Learn from Listening” | Anne Gosline is the Executive Director of the Massachusetts Coalition for Serious Illness Care and a Senior Director in the Executive Office of Blue Cross |
|
|
|
|
|
| “Microaggressions and its Macro-impact: Surviving Difficult Spaces” | Kimberly Angelia Curseen, MD is the Director of Outpatient Supportive Care; Emory Palliative Care Center, and the Director of Winship Palliative Medicine Program.
|
|
| Registration Type | Tuition Price |
|---|---|
| All Healthcare Providers | $250.00 |
For questions regarding the registration process, please contact Mass General Brigham Office of Continuing Professional Development at mgbcpd@mgb.org.
Group Discounts
We encourage teams to enroll in this course together and to benefit from the shared experience and from gaining a common language for palliative care and geriatric medicine. Group discounts are available:
- 10% discount for enrolling 10-19 learners
- 20% discount for enrolling 20-29 learners
- 30% discount for enrolling 30 or more learners
Please contact the HMS Center for Palliative Care at pallcare@partners.org to register a group.
If you register a group of 20 or more, you can apply for up to two live 1-hour discussion sessions via Zoom with a member of the HMS CPC faculty. Additional information will be provided subsequent to your registration.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => 1 [field_target_audience] => Array ( [value] =>The MGH Palliative Care and Geriatric Medicine Grand Rounds series is unique in its design for all of the interprofessional members of a palliative care team, including Physicians, Nurse Practitioners, Physician Assistants, Psychiatrists, Psychologists, Nurses, Social Workers, and Chaplains.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3545 [id] => 3545 [resource] => accme_data ) [field_show_on_calendar] => [field_custom_provided] => Array ( [value] =>
[summary] => [format] => full_html ) [field_course_exhibitor] => Array ( ) [field_course_qualifiers] => Array ( ) [field_course_image_cards] => Array ( ) [field_income_expense] => Array ( ) [og_membership] => Array ( ) [og_membership__1] => Array ( ) [og_membership__2] => Array ( ) [og_membership__3] => Array ( ) [og_group_ref__og_membership] => Array ( ) [og_group_ref__og_membership__1] => Array ( ) [og_group_ref__og_membership__2] => Array ( ) [og_group_ref__og_membership__3] => Array ( ) [flag_course_bookmark_user] => Array ( ) [model] => course_81317 [list_price] => 0.00000 [cost] => 0.00000 [sell_price] => 250.00000 [price] => 250.00000 [weight] => 0 [weight_units] => lb [length] => 0 [width] => 0 [height] => 0 [length_units] => in [pkg_qty] => 1 [ordering] => 0 [shippable] => 0 [nid] => 81317 [vid] => 229610 [is_new] => [type] => course [title] => MGH Palliative Care and Geriatric Medicine Grand Rounds Course Bundle [language] => und [url] => https://cpd.partners.org/content/mgh-palliative-care-and-geriatric-medicine-grand-rounds-course-bundle [edit_url] => https://cpd.partners.org/node/81317/edit [status] => 1 [promote] => 0 [sticky] => 0 [created] => 1729539425 [changed] => 1747831729 [author] => Array ( [uri] => https://cpd.partners.org/user/257 [id] => 257 [resource] => user [uuid] => bd6fd397-09cf-4275-a7d4-35783f50f323 ) [log] => [revision] => [course] => Array ( [uri] => https://cpd.partners.org/course/81317 [id] => 81317 [resource] => course ) [book_ancestors] => Array ( ) [comment] => 1 [comments] => Array ( ) [comment_count] => 0 [comment_count_new] => 0 [body] => Array ( ) [feeds_item_guid] => [feeds_item_url] => [feed_nid] => [relation_faculty_user] => Array ( ) [uuid] => b4bfb635-a0f0-4ec9-8bbf-0d0a0baf16b0 [vuuid] => 3fc91306-4e97-4818-b213-2ac831cdfc18 ) ) )
Array
(
[self] => https://cpd.partners.org/node?nid=54410
[first] => https://cpd.partners.org/node?nid=54410&page=0
[last] => https://cpd.partners.org/node?nid=54410&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => Accreditation
In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 Credits™
Mass General Brigham designates this live activity for a maximum of 8 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 8 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
Physician Assistants
Mass General Brigham has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 8 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation.

MOC COMPLETION CRITERIA
Participant completion for MOC points will be reported to the boards at the conclusion of the course.
Please have your ABIM ID available when completing the evaluation at the end of the course.
Instructions: Medical Knowledge MOC points in the American Board of Internal Medicine's (ABIM) Maintenance of Certification (MOC) Program
Upon successful completion of this activity, if you wish to receive MOC Part 2 points you will need to enter your ABIM ID number in the post-course evaluation. The Mass General Brigham Office of Continuing Professional Development will verify completion of your activity and report to the ABIM. Diplomates must check their ABIM Portfolio for confirmation of your MOC Part 2 points.
MOC Recognition Statement
Successful completion of this CME activity, which includes participation in the activity, with individual assessments of the participant and feedback to the participant, enables the participant to earn 8 MOC points in the American Board of Internal Medicine (ABIM) Maintenance of Certification (MOC) program. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/197
[id] => 197
[resource] => taxonomy_term
[uuid] => 621a8034-627c-4c33-b273-260b2d83768c
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1666205160
[value2] => 1682049540
[duration] => 15844380
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1678708800
[value2] => 1678741200
[duration] => 32400
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/239
[id] => 239
[resource] => taxonomy_term
[uuid] => 8fe8f562-9596-41a9-8e2f-c93aa2c8dae9
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/38857
[id] => 38857
[resource] => file
[uuid] => bf3dd6fa-9e9b-406c-9643-1d4dcca012e1
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 31396
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Livestream
[street] => The Massachusetts General Hospital
[additional] =>
[city] => Boston
[province] => MA
[postal_code] => 02114
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => 
Monday, March 13, 2023
8:00am - 5:00pm
Livestream
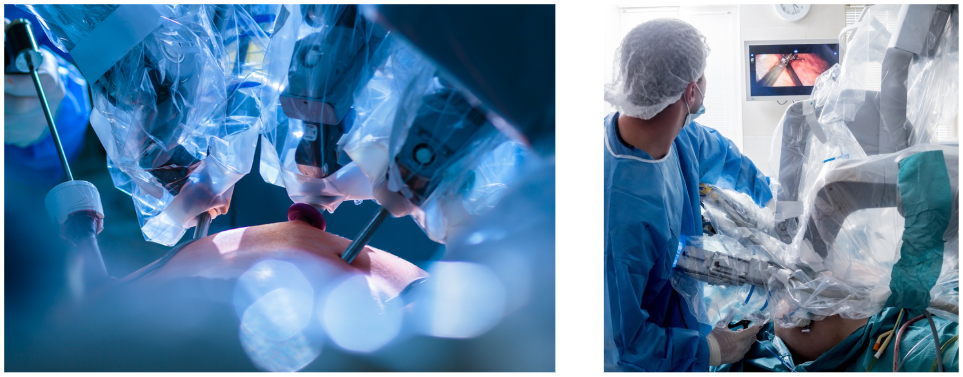
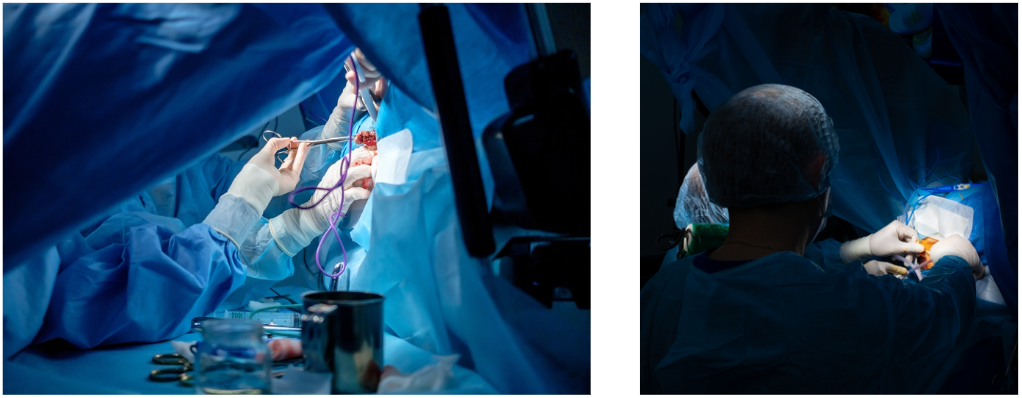
This course provides interactive didactic lectures and video demonstration of management approaches in the multidisciplinary care of patients with acute heart and lung failure. While there are other CME courses offered at regional academic centers, no center offers an integrated course on heart and lung support.
Our Short-term MCS course brings together a uniquely multidisciplinary panel of speakers, not only including cardiologists, cardiothoracic surgeons and pulmonologists, but also respiratory therapists, nurses and palliative care physicians. The course faculty reflects the complexity of care for patients with acute heart and lung failure and illustrates how a team of diverse providers work together to address challenges to improve quality of care.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Course Co-Directors
Van-Khue Ton, MD, PhD

Assistant Professor of Medicine, Harvard Medical School;
Advanced Heart Failure & Transplantation Cardiologist, Massachusetts General Hospital
Jerome Crowley, MD, MPH

Instructor in Anesthesia, Harvard Medical School;
Cardiothoracic Anesthesiologist, Critical Care Medicine, Massachusetts General Hospital
Eriberto Michel, MD



Assistant Professor of Surgery, Harvard Medical School;
Cardio-Thoracic Surgeon, Massachusetts General Hospital
Jona Ludmir, MD
Assistant Professor of Medicine, Harvard Medical School;
Critical Care Cardiologist, Massachusetts General Hospital
Faculty
Erin Coglianese, MD
Assistant Professor of Anesthesia, Harvard Medical School;
Medical Director, Mechanical Cardiac Support, Massachusetts General Hospital
David Convissar, MD
Instructor in Anesthesia, Harvard Medical School;
Anesthesiologist, Critical Care and Pain Medicine, Massachusetts General Hospital
Gaston Cudemus, MD
Chief, Cardiac Anesthesiology and Medical Director of ECMO Program, NCH Heart Institute
David D'Alessandro, MD
Associate Professor of Surgery, Harvard Medical School;
Surgical Director, Heart Transplantation and Ventricular Assist Devices, Massachusetts General Hospital
Danielle Doucette, BS, RT
ECMO Coordinator, Cardiology Division, Massachusetts General Hospital
David Dudzinksi, MD
Assistant Professor of Medicine, Harvard Medical School;
Director of Cardiac Intensive Care Unit, Massachusetts General Hospital
Navin Kapur, MD, FAHA, FACC, FSCAI
Associate Professor, Tufts University School of Medicine;
Director, Acute Mechanical Circulatory Support Program, Tufts University School of Medicine
Yvonne Lai, MD
Assistant Professor of Anesthesia, Harvard Medical School;
Anesthesiologist, Critical Care Medicine, Massachusetts General Hospital
Christine McCarthy, CNP
Nurse Practitioner, Palliative Care and Geriatric Medicine, Massachusetts General Hospital
Kamal Medlej, MD
Instructor in Emergency Medicine, Harvard Medical School;
Emergency Medicine Specialist, Critical Care Physician, Massachusetts General Hospital
Ivana Nikoli, MD
Instructor in Medicine, Harvard Medical School;
Cardiologist, Massachusetts General Hospital
Ali Pitti, CCP, LP, MS
Senior Perfusionist, Massachusetts General Hospital
Emily Rubin, MD
Instructor in Medicine, Harvard Medical School;
Pulmonary and Critical Care Physician, Massachusetts General Hospital
Jonah Rubin, MD
Instructor in Medicine, Harvard Medical School;
Critical Care Physician and Pulmonologist, Massachusetts General Hospital
Kenneth Shelton, MD
Assistant Professor of Anesthesia, Harvard Medical School;
Chief, Division of Critical Care, Massachusetts General Hospital
Alyssa Taubert, OT, OTD, OTR, CBIS
Doctor of Occupational Therapy, Massachusetts General Hospital
Mauricio Villavicencio, MD
Associate Professor of Surgery, Mayo Clinic College of Medicine;
Surgical Director of Heart & Lung Transplantation and Mechanical Circulatory Support, Mayo Clinic
Alison Witkin, MD
Assistant Professor of Medicine, Harvard Medical School;
Associate Director of Pulmonary Hypertension and Thromboendarterectomy, Massachusetts General Hospital
Sarah D. Wright, PT
Board Certified Cardiovascular and Pulmonary Clinical Specialist,
Doctor of Physical Therapy, Massachusetts General Hospital
Adil Yunis, MD
Cardiology Clinical Fellow, Harvard Medical School;
Cardiology Division, Massachusetts General Hospital
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Describe an Extracorporeal membrane oxygenation (ECMO) circuit including pumps, filters, tubing, safety monitors, oxygenators, heating and cooling elements, and different variations in the set up.
- Recognize and explain the different types of cannulae and cannulation strategies for ECMO.
- Recognize and manage cardiogenic shock.
- Identify and manage acute lung failure.
- Recognize the indications for TCS devices (heart pumps, cannula devices, and ECMO).
- Diagnose and manage common complications associated with ECMO and other TCS devices.
- Interpret hemodynamic data for patients with short-term support.
- Evaluate and manage weaning from ECMO and other short term support.
- Demonstrate the importance of involving Palliative Care and Ethics in the management of acute heart and lung failure.
- Describe the steps in building a multidisciplinary team.
- Describe physical therapy strategies to mobilize and “pre-hab” patients on short term support while waiting for heart and lung transplant.
- Describe the role of heart transplant and durable mechanical circulatory support in the care of patients with cardiogenic shock.
- Determine the latest development of heart and lung support devices in the pipeline.
Social Media
Twitter:
Mass General Brigham Professional Development
@MassGenBrighCPD
MGH Corrigan Minehan Heart Center
@MGHHeartHealth
LinkedIn:
Mass General Brigham Professional Development
[format] => full_html
)
[field_program] => Array
(
[value] => PART 1 (Morning): | |
| 8:00am | Welcome & Introduction | Van-Khue Ton, MD, PhD; Jerome Crowley, MD, MPH; Eriberto Michel, MD; Jona Ludmir, MD |
Act 1: Cardiogenic Shock & Temporary Circulatory Support | |
| 8:05 | Keynote Presentation: Recent Advances in Cardiogenic Shock Treatment | Navin Kapur, MD |
| 8:25 | Rationale Behind Temporary Circulatory Support | Van-Khue Ton, MD, PhD |
| 8:40 | ECMO: Circuits & Basic Trouble Shooting | Ali Disanto & Danielle Doucette, RT |
| 8:55 | ECMO: Selection Criteria – Indication, Contraindications, Risk Stratification | David Convissar, MD |
| 9:10 | Panel Q&A |
| 9:25 | BREAK |
| 9:30 | 3 Case Study Presentations with Q&A and Polling |Presented by Fellows; Moderated by Van-Khue Ton, MD, PhD; Jerome Crowley, MD, MPH; Eriberto Michel, MD; Jona Ludmir, MD |
| 10:15 | BREAK |
Act 2: All of the Bridges | |
| 10:25 | How and When to Wean Temporary MCS | Jona Ludmir, MD |
| 10:40 | Transition from Temporary to Durable MCS | Erin Coglianese, MD |
| 11:10 | When You Can't Wean | Christine McCarthy, MD & Emily Rubin, MD |
| 11:25 | Panel Q & A |
| 11:40 | LUNCH BREAK |
PART 2 (Afternoon): | |
| 12:20pm | Welcome Back! | Van-Khue Ton, MD, PhD; Jerome Crowley, MD, MPH; Eriberto Michel, MD; Jona Ludmir, MD |
Act 1: Lungs | |
| 12:25 | Severe ARDS: Considerations for Veno-venous ECMO | Alison Witkin, MD |
| 12:40 | Non-ARDS indications for VV ECMO | Jonah Rubin, MD |
| 12:55 | Massive PE: Considerations for ECMO | Ivana Nikolic, MD |
| 1:10 | Transitioning From Short-Term Support to Lung Transplant | Eriberto Michel, MD |
| 1:25 | Panel Q&A |
| 1:40 | BREAK |
| 1:45 | 3 Case Study Presentations with Q&A and Polling | Presented by Fellows; Moderated by Van-Khue Ton, MD, PhD; Jerome Crowley, MD, MPH; Eriberto Michel, MD; Jona Ludmir, MD |
| 2:30 | BREAK |
Act 2: Advanced Clinical Management | |
| 2:35 | ECMO 102: Beyond the Basics | Jerome Crowley, MD |
| 2:50 | Post-Cardiotomy Shock | Yvonne Lai, MD |
| 3:05 | Innovative Approaches to “Pre-Habbing” Patients on Temporary Support | Sarah Wright, PT DPT CCS & Alyssa Taubert, OT, OTD, OTR, CBIS |
| 3:20 | Panel Q&A |
| 3:35 | BREAK |
Act 3: Moving Forward - Future of Temporary Heart/Lung Support | |
| 3:40 | Building a Multidisciplinary Team (combined talk) | Kamal Medlej, MD & Gaston Cudemus, MD |
| 3:55 | Medicolegal Risks of Temporary Support | David Dudzinski, MD, JD |
| 4:10 | Over the Horizon: Temporary Heart/Lung Support in the Pipeline | Mauricio Villavicencio, MD |
| 4:25 | Panel Q&A |
| 4:35 | Complex Case Presentation (ECMO CPC) | Adil Yunis, MD; Kenneth Shelton, MD; Van-Khue Ton, MD, PhD; Jerome Crowley, MD, MPH; Eriberto Michel, MD; Jona Ludmir, MD |
| 4:55 | Closing Remarks | Van-Khue Ton, MD, PhD; Jerome Crowley, MD, MPH; Eriberto Michel, MD; Jona Ludmir, MD |
| 5:00pm | Adjourn |
[format] => full_html ) [field_registration_instructions] => Array ( [value] =>
| Registration type | Early Bird Rate (Before February 20th) | Standard Rate (After February 20th) |
|---|---|---|
| General Tuition | $150.00 | $175.00 |
| Fellows | $50.00 | $50.00 |
Cancellation Policy:
Registrations cancelled on or before February 27, 2023 will be refunded, less a $20 administrative fee. Registrations cancelled after February 27, 2023 will not be refunded.
Contact partnerscpd@partners.org if you require assistance in cancelling your online registration.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for physicians, nurses, and physician assistants in Anesthesiology, Cardiac Surgery, Cardiology, Critical Care, Hospice and Palliative Care, Internal Medicine, Interventional Cardiology, Pulmonary Disease.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/2421 [id] => 2421 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital - Corrigan Minehan Heart Center and
Mass General Brigham
[summary] => [format] => full_html ) [field_course_exhibitor] => Array ( ) [field_course_qualifiers] => Array ( ) [field_course_image_cards] => Array ( ) [field_income_expense] => Array ( ) [og_membership] => Array ( ) [og_membership__1] => Array ( ) [og_membership__2] => Array ( ) [og_membership__3] => Array ( ) [og_group_ref__og_membership] => Array ( ) [og_group_ref__og_membership__1] => Array ( ) [og_group_ref__og_membership__2] => Array ( ) [og_group_ref__og_membership__3] => Array ( ) [flag_course_bookmark_user] => Array ( [0] => Array ( [uri] => https://cpd.partners.org/user/103126 [id] => 103126 [resource] => user [uuid] => 2ac844bf-147b-429b-b54b-d429de64fa7a ) [1] => Array ( [uri] => https://cpd.partners.org/user/103047 [id] => 103047 [resource] => user [uuid] => 2e765a35-2c39-49fc-ab96-d19f0ecc3f55 ) [2] => Array ( [uri] => https://cpd.partners.org/user/97957 [id] => 97957 [resource] => user [uuid] => 076b7180-113a-407f-85c0-7709db1710ef ) [3] => Array ( [uri] => https://cpd.partners.org/user/102621 [id] => 102621 [resource] => user [uuid] => 150ceed5-ea30-45e0-8db9-80476ba44098 ) [4] => Array ( [uri] => https://cpd.partners.org/user/99825 [id] => 99825 [resource] => user [uuid] => 1241713c-63cf-4a04-8f4b-8a1e68ee5495 ) [5] => Array ( [uri] => https://cpd.partners.org/user/98075 [id] => 98075 [resource] => user [uuid] => d5e2ab83-3145-4d83-91be-d4bb8dcab6a1 ) [6] => Array ( [uri] => https://cpd.partners.org/user/90769 [id] => 90769 [resource] => user [uuid] => fec1ddab-5d6a-4b28-b4e7-927c539d833c ) ) [model] => course_54410 [list_price] => 0.00000 [cost] => 0.00000 [sell_price] => 175.00000 [price] => 175.00000 [weight] => 0 [weight_units] => lb [length] => 0 [width] => 0 [height] => 0 [length_units] => in [pkg_qty] => 1 [ordering] => 0 [shippable] => 0 [nid] => 54410 [vid] => 150360 [is_new] => [type] => course [title] => Short Term Mechanical Support Heart and Lung Symposium 2023 [language] => und [url] => https://cpd.partners.org/content/HeartandLungSymposium2023 [edit_url] => https://cpd.partners.org/node/54410/edit [status] => 1 [promote] => 1 [sticky] => 1 [created] => 1666208797 [changed] => 1681500293 [author] => Array ( [uri] => https://cpd.partners.org/user/92 [id] => 92 [resource] => user [uuid] => 48adffb8-b573-4cd5-ada8-52d9bb7f0770 ) [log] => [revision] => [course] => Array ( [uri] => https://cpd.partners.org/course/54410 [id] => 54410 [resource] => course ) [book_ancestors] => Array ( ) [comment] => 1 [comments] => Array ( ) [comment_count] => 0 [comment_count_new] => 0 [body] => Array ( ) [feeds_item_guid] => [feeds_item_url] => [feed_nid] => [relation_faculty_user] => Array ( ) [uuid] => 37df2902-23be-4051-8f4c-3b489865cbb0 [vuuid] => a5f4543e-729f-447e-bab8-a9d2f64bcf50 ) ) )
Array
(
[self] => https://cpd.partners.org/node?nid=57074
[first] => https://cpd.partners.org/node?nid=57074&page=0
[last] => https://cpd.partners.org/node?nid=57074&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => enrolled
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Mass General Brigham designates this live activity for a maximum of 22.25 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/234
[id] => 234
[resource] => taxonomy_term
[uuid] => d2fa0dc6-c937-4cce-88aa-496b736f4bbc
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1680870600
[value2] => 1708145940
[duration] => 27275340
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1697255940
[value2] => 1697403600
[duration] => 147660
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/7
[id] => 7
[resource] => taxonomy_term
[uuid] => 2a38b69f-4c76-44b0-bde5-67e901205c53
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/47957
[id] => 47957
[resource] => file
[uuid] => ed0c01cd-631f-45b9-bf7c-56af43c95ba5
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => This is a fully virtual event
Description
For more than 40 years, “Advances in Rheumatology” has been influential in educating generations of clinicians on over 100 rheumatic conditions, which now encompass the specialty. A collaboration between Harvard Medical School’s two largest teaching hospitals, the Massachusetts General Hospital and Brigham and Women’s Hospital, the course not only focuses on rheumatic diseases, but offers additional perspectives from other medical disciplines, such as pulmonology, dermatology, oncology, ophthalmology, and endocrinology. “Advances in Rheumatology” targets the practicing clinician seeking to enhance their clinical skills and increase their knowledge with the latest breakthroughs in the diagnosis, treatment, and pathophysiology of rheumatic diseases.
This three day livestream course will be a combination of sessions formatted with lectures by leading experts on topics pertaining to their special areas of interest, curbside consultations and panel discussions. Topics include The Year in Rheumatology, updates on Giant Cell Arteritis, Orbital Inflammatory Disease, Systemic Sclerosis, Hemophagocytic Syndrome, the New England Journal of Medicine Clinicopathological Conference (CPC) and various disease focused afternoon sessions such as Lupus, Psoriatic Arthritis and Rheumatoid Arthritis. The full range of rheumatic disease is covered every year over the span of this course.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Advances in Rheumatology Course Directors
John H. Stone, MD, MPH
Professor of Medicine, Harvard Medical School;
The Edward A. Fox Chair in Medicine, Massachusetts General Hospital
Michael Weinblatt, MD
John R. Riedman Professor of Medicine, Harvard Medical School;
Co-Director, Clinical Rheumatology,
Associate Director, Center for Arthritis and Joint Diseases,
Brigham and Women’s Hospital
Advances in Rheumatology Speakers
Rohit Aggarwal MD, MS
University of Pittsburgh
Luke Chen, MD
BC Cancer | Vancouver, BC
Stanley Cohen, MD
Christian Dejaco, MD
Brunico Hospital
Atul Deodhar, MD
Oregon Health & Science University
Thomas Dorner, MD
Charite University Hospital
David Dudzinski, MD, JD
Massachusetts General Hospital
Paul Emery, MD
University of Leeds
Judith Ferry, MD
Massachusetts General Hospital
Ambrose Huang, MD
Massachusetts General Hospital
Laura Hummers, MD
Johns Hopkins University
David Isenberg, MD, FRCP, FAMS
University College London
Michael Jordan, MD
Cincinnati Children’s Hospital
Andreas Kronbichler, MD
Medical University Innsbruck
Katherine Liao, MD
Brigham and Women’s Hospital
Andrew Mammen, MD, PhD
National Institute of Health
Iain B McInnes, CBE, PhD, FRCP, FRSE, FMedSci.
University of Glasgow
Joseph Merola, MD
Brigham and Women’s Hospital
Alexis Ogdie, MD, MSCE
University of Pennsylvania
Julie Paik, MD
Johns Hopkins University
Michelle Petri, MD, MPH
Johns Hopkins University
Brad Rovin, MD
Ohio State University
Ami Shah, MD
Johns Hopkins University
Allen Steere, MD
Massachusetts General Hospital
Ronald van Vollenhofen, MD
University of Amsterdam
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of Advances in Rheumatology, participants will be able to:
- Evaluate the latest scientific advances in the field of rheumatology.
- Analyze insights from pathology, immunology, and pharmacology that pertain to specific rheumatologic issues.
- Translate the latest developments in the field of rheumatology to clinical practice.
- Integrate new treatment approaches for patients with rheumatic disease.
- Apply new diagnostic techniques in their patient population.
MOC Completion Criteria
Participant completion for MOC points will be reported to the boards at the conclusion of the course.
Please have your ABIM ID available when completing the evaluation at the end of the course.
Instructions: Medical Knowledge MOC points in the American Board of Internal Medicine's (ABIM) Maintenance of Certification (MOC) Program
Upon successful completion of this activity, if you wish to receive MOC Part 2 points you will need to enter your ABIM ID number in the post-course evaluation. The Mass General Brigham Office of Continuing Professional Development will verify completion of your activity and report to the ABIM. Diplomates must check their ABIM Portfolio for confirmation of your MOC Part 2 points.
MOC Recognition Statement
Successful completion of this CME activity, which includes participation in the activity, with individual assessments of the participant and feedback to the participant, enables the participant to earn 22.25 MOC points in the American Board of Internal Medicine (ABIM) Maintenance of Certification (MOC) program. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
Funding
Advances in Rheumatology 2023 has received support in the form of an educational grant from the following companies:
AstraZeneca Pharmaceuticals
Bristol Myers Squibb
Janssen Biotech,Inc., administered by Janssen Scientific Affairs, LLC
Novartis
[format] => full_html
)
[field_program] => Array
(
[value] => Friday, October 13, 2023 | 7:00am - 5:00pm
| 7:00am | Registration for Advances in Rheumatology |
| 7:30 | The Year in Clinical Rheumatology | John H. Stone, MD, MPH |
| 8:30 | Giant Cell Arteritis & Polymyalgia Rheumatica: Answering the Currently Critical Questions | Christian Dejaco, MD, PhD, MBA |
| 9:30 | Morning Break |
| 9:45 | ANCA-Associated Vasculitis: The Nephrologist’s Perspective | Andreas Kronbichler, MD |
| 10:45 | New England Journal of Medicine Clinicopathologic Conference | Luke Chen, MD; John H. Stone, MD, MPH; Ambrose Huang, MD; Judith Ferry, MD; David Dudzinski, MD, JD |
| 12:00pm | Lunch |
Disease Focused Afternoon Session: Lupus Nephritis | |
| 1:00 | Important Clinical Outcomes in SLE: How are we doing now? | Michelle Petri, MD, MPH |
| 1:45 | B Cell Depletion in Lupus: How will it fit into the current treatment paradigms? | David Isenberg, MD, FRCP, FAMS |
| 2:15 | Break |
| 2:30 | Calcineurin Inhibitors in SLE Nephritis | Brad Rovin, MD |
| 3:00 | Novel Treatment Approaches to Lupus | Thomas Dorner, MD |
| 3:30 | Break |
| 3:45 | Panel Discussion | Michelle Petri, MD MPH; David Isenberg, MD; Brad Rovin, MD; Thomas Dorner, MD |
| 5:00pm | Adjourn |
Saturday, October 14, 2023 | 7:45am - 4:30pm
| 7:45am | Log-In Time |
| 8:00 | The Pathologies of Inflammatory Myopathy | Andrew Mammen, MD, PhD |
| 8:45 | Using Autoantibodies to Parse the Inflammatory Myopathies | Julie Paik, MD |
| 9:45 | Morning Break |
| 10:15 | Difficult Myopathies | Rohit Aggarwal, MD, MS |
| 11:00 | Challenges in Lyme Disease | Allen Steere, MD |
| 12:00pm | Lunch |
Disease Focused Afternoon Session: Psoriasis & Psoriatic Arthritis | |
| 1:00 | Important Outcomes in Psoriasis/ Psoriatic Arthritis: How are we doing now? | Alexis Ogdie, MD, MSCE |
| 1:30 | How does a Rheumatologist approach Psoriasis Treatment? | Joseph Merola, MD |
| 2:00 | Break |
| 2:15 | Treatment of PsA | Iain B McInnes, CBE, PhD, FRCP, FRSE, FMedSci. |
| 2:45 | Treatment of Spondylitis | Atul Deodhar, MD |
| 3:15 | Break |
| 3:30 | Panel Discussion | Joseph Merola, MD; Iain B McInnes, CBE, PhD, FRCP, FRSE, FMedSci.; Atul Deodhar, MD; Alexis Ogdie, MD, MSCE |
| 4:30pm | Adjourn |
Sunday, October 15, 2023 | 7:15am - 5:00pm
| 7:15am | Log-In |
| 7:30 | Tackling Diffuse Systemic Sclerosis | Ami Shah, MD |
| 8:30 | How to Approach Limited Scleroderma Now | Laura Hummers, MD |
| 9:30 | Morning Break |
| 9:45 | Identifying & Treating the Hemophagocytic Syndrome | Michael Jordan, MD |
| 10:45 | A Practical Tour through IgG4-Related Disease: Lessons from the patients over 15 years | John H. Stone, MD, MPH |
| 11:45 | Lunch |
Disease Focused Afternoon Session: Rheumatoid Arthritis | |
| 1:00pm | Important Outcomes in RA: How are we doing now? | Katherine Liao, MD |
| 1:30 | Methotrexate in Rheumatoid Arthritis | Michael Weinblatt, MD |
| 2:00 | Break |
| 2:15 | Biologics and Jak Inhibition | Ronald van Vollenhofen, MD |
| 2:45 | How does a Rheumatologist approach RA Treatment? (Europe & USA) | Paul Emery, MD (Europe) & Stanley Cohen, MD (Southwestern USA) |
| 3:45 | Break |
| 4:00 | Panel Discussion | Katherine Liao, MD; Ronald Von Vollenhofen, MD; Paul Emery, MD; Stanley Cohen, MD |
| 5:00pm | Adjourn |
[format] => full_html ) [field_registration_instructions] => Array ( [value] =>
This is a fully virtual event
| Registration Type | Full Registration Fee |
|---|---|
| Physician | $600.00 |
| Resident/Fellow | $150.00 |
| Nurse | $300.00 |
| Other Allied Healthcare Professionals (Pharmacists, Physician Assistants, PhD) | $300.00 |
| Industry | $800.00 |
Cancellation Policy:
Registrations cancelled on or before September 29, 2023 will be refunded, less a $60 administrative fee. Registrations cancelled after September 29, 2023 will not be refunded.
Contact partnerscpd@partners.org if you require assistance in cancelling your online registration.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>
This activity is intended for Primary Care Physicians, Specialty Physicians, Nurse Practitioners, Physician Assistants, Dermatology, Endocrinology, Family Medicine, Infectious Disease, Internal Medicine, Oncology and Hematology, Ophthalmology, Orthopedics, Pathology, Preventative Medicine, Pulmonary Medicine, Rheumatology, Urology, Allergy and Immunology.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/2665 [id] => 2665 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital, Brigham and Women's Hospital, & Mass General Brigham
[summary] => [format] => full_html ) [field_course_exhibitor] => Array ( ) [field_course_qualifiers] => Array ( ) [field_course_image_cards] => Array ( ) [field_income_expense] => Array ( ) [og_membership] => Array ( ) [og_membership__1] => Array ( ) [og_membership__2] => Array ( ) [og_membership__3] => Array ( ) [og_group_ref__og_membership] => Array ( ) [og_group_ref__og_membership__1] => Array ( ) [og_group_ref__og_membership__2] => Array ( ) [og_group_ref__og_membership__3] => Array ( ) [flag_course_bookmark_user] => Array ( [0] => Array ( [uri] => https://cpd.partners.org/user/75350 [id] => 75350 [resource] => user [uuid] => 3786a953-b85c-48b8-803c-0a0371f9a939 ) ) [model] => course_57074 [list_price] => 0.00000 [cost] => 0.00000 [sell_price] => 600.00000 [price] => 600.00000 [weight] => 0 [weight_units] => lb [length] => 0 [width] => 0 [height] => 0 [length_units] => in [pkg_qty] => 1 [ordering] => 0 [shippable] => 0 [nid] => 57074 [vid] => 184856 [is_new] => [type] => course [title] => Advances in Rheumatology 2023 [language] => und [url] => https://cpd.partners.org/content/advances-rheumatology-2023 [edit_url] => https://cpd.partners.org/node/57074/edit [status] => 1 [promote] => 1 [sticky] => 1 [created] => 1680870724 [changed] => 1707752197 [author] => Array ( [uri] => https://cpd.partners.org/user/92 [id] => 92 [resource] => user [uuid] => 48adffb8-b573-4cd5-ada8-52d9bb7f0770 ) [log] => [revision] => [course] => Array ( [uri] => https://cpd.partners.org/course/57074 [id] => 57074 [resource] => course ) [book_ancestors] => Array ( ) [comment] => 1 [comments] => Array ( ) [comment_count] => 0 [comment_count_new] => 0 [body] => Array ( ) [feeds_item_guid] => [feeds_item_url] => [feed_nid] => [relation_faculty_user] => Array ( ) [uuid] => 0eb830ad-d608-46d7-873a-17f029df4fbb [vuuid] => 1058a122-31c3-45c1-a4c9-efa5303c054c ) ) )
Array
(
[self] => https://cpd.partners.org/node?nid=55070
[first] => https://cpd.partners.org/node?nid=55070&page=0
[last] => https://cpd.partners.org/node?nid=55070&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this live activity for a maximum of 13.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 13.5 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/231
[id] => 231
[resource] => taxonomy_term
[uuid] => 541dec03-c6af-4bcb-9af7-8fa28fedfb53
)
[1] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/232
[id] => 232
[resource] => taxonomy_term
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1670245200
[value2] => 1686369540
[duration] => 16124340
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1682078400
[value2] => 1682197200
[duration] => 118800
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/4
[id] => 4
[resource] => taxonomy_term
[uuid] => c57cf9bf-73d6-4eaa-9f35-e4e9cce75d36
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/42895
[id] => 42895
[resource] => file
[uuid] => 8566edb6-cd14-4380-b7c2-8ac48ed9bbec
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 32595
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Boston Marriott Cambridge
[street] => 50 Broadway
[additional] =>
[city] => Cambridge
[province] => MA
[postal_code] => 02142
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] =>

This is a hybrid event
Now more than ever, the presence of social inequities in healthcare is evident. This two-day, hybrid event, the Cancer Equity Colloquium, will address the diverse issues that underlie cancer inequities. The goal of the Colloquium is to bring together individuals from healthcare, academia, private/public business sector, and the public at large to develop unique approaches to tackling these inequities. We know that impactful initiatives to promote cancer equity require the skills and experiences of individuals from all these sectors of society. The speakers will reflect a similar mixture of backgrounds. Attendees will have the opportunity to engage with each other and the Cancer Equity Colloquium faculty in hopes to develop novel partnerships.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Course Co-Directors
Colin D. Weekes, MD, PhD
Christopher D. Horner Endowed Chair in Pancreatic Cancer,
Director, Pancreatic Cancer Research,
Director, Cancer Center Grand Rounds,
Massachusetts General Hospital Cancer Center;
Associate Professor of Medicine, Harvard Medical School
Brenda Lormil, MSN, FNP-C
Nurse Practitioner, Massachusetts General Hospital Cancer Center;
Founder, Haitian American Medical Association (HAMA)
Speakers
Michele Barber, MS, GNP-BC, AOCNP
Associate Director, Oncology Patient Engagement, Alkermes;
Director-at-large, Boston Oncology Nursing Society (BONS)
A. William Blackstock Jr., MD
Chair, Radiation Oncology,
Interim Director, Comprehensive Cancer Center,
Atrium Health Wake Forest Baptist
Karen Burns White
Deputy Associate Director, Initiative to Eliminate Cancer Disparities,
Dana-Farber / Harvard Cancer Center
Cesar Castro, MD
Program Director, Gynecologic Oncology
Massachusetts General Hospital Cancer Center
Taneshia Camillo-Sheffey
Consultant, Founder & Director,
The Haute House Design Studio
MadelNcubator, Inc
Crystal Davis, RN
Registered Nurse,
Beth Israel Deaconess Medical Center
Neelima Denduluri, MD, FASCO
Global Clinical Head, Late Phase Research & Development,
AstraZeneca
Cesar Depaz
Senior Pastor, Hispanic Community Church of Boston
Clifton David Fuller, MD, PhD
Professor, Division of Radiation Oncology,
The University of Texas MD Anderson Cancer Center
S. Autumn Gaston, BSN, RN
Infusion Nurse, Termeer Center,
Massachusetts General Hospital Cancer Center
Rev. Deborah Hamilton, MDiv, BSN, RN, FCN
Lecturer, Dept. of Health Sciences (part-time), Northeastern University;
Staff Chaplain, Boston Medical Center (part-time)
Nora Hathaway, NP
Inpatient Medical Oncology,
Massachusetts General Hospital Cancer Center
Natasha Gross Jean, RN, BSN, OCN
Hematology Clinic Infusion Center,
Boston Medical Center
Christopher Lathan, MD, MS, MPH
Chief Clinical Access and Equity Officer, Dana-Farber Cancer Institute;
Christopher and Constance Hadley Family Chair at Dana Farber;
Associate Chief Medical Officer, Director, Dana-Farber Cancer Institute Network;
Associate Professor of Medicine, Harvard Medical School
Lisa Lewis, MPH
Director, Diversity, Equity and Inclusion in Clinical Trials,
Janssen Oncology
Rev. Jean J.M. Louis
Senior Pastor, Free Pentecostal Church of God
Meghan McKenzie, MA
Principal, Patient Inclusion & Health Equity,
Chief Diversity Office, Genentech
Ruben A. Mesa, MD, FACP
Senior Vice President, Atrium Health;
President, Cancer Service Line, Atrium Health;
Executive Director, Atrium Health Wake Forest Baptist Comprehensive Cancer Center;
Vice Dean for Cancer Programs, Wake Forest School of Medicine
Edith P. Mitchell, MD, MACP, FCPP, FRCP (London)
Clinical Professor of Medicine and Medical Oncology,
Department of Medical Oncology,
Enterprise Vice President for Cancer Disparities,
Director, Center to Eliminate Cancer Disparities,
Associate Director, Diversity Affairs
Sidney Kimmel Cancer Center at Jefferson
Mike Moise, MSA, CPA
Director of Finances, Haitian America Medical Association;
Associate Director, Life Sciences Practice, CrossCountry Consulting
Jean Claude Noel, MS, MA
Atrium Consulting LLC - New York
Kets de Vries Institute - London
European Foundation for Management Development - Brussels
Mount Sinai Hospital Tisch Cancer Institute - New York
Boston Graduate School of Psychoanalysis - Boston
Olorunseun (Seun) Ogunwobi, MD, PhD
Director, Hunter College Center for Cancer Health Disparities Research (CCHDR);
Professor of Biological Sciences, Hunter College of The City University of New York
Raymond Osarogiagbon, MD, FACP
Chief Scientist,
Baptist Memorial Health Care Corporation;
Director, Multidisciplinary Thoracic Oncology Program,
Baptist Cancer Center
Electra D. Paskett, PhD
Marion N. Rowley Professor of Cancer Research,
Director, Division of Cancer Prevention and Control, College of Medicine;
Professor, Division of Epidemiology, College of Public Health;
Associate Director for Population Sciences and Community Outreach,
Comprehensive Cancer Center
The Ohio State University
Founding Director, Center for Cancer Health Equity, James Cancer Hospital
Kenley Preval
MD/PhD Student, UMass Medical School
Stanley Rameau
Founder & CEO, Renavest;
Founder & CEO, Paul Rameau
Jamie L. Studts, PhD
Professor, Division of Medical Oncology,
Scientific Director, Behavioral Oncology,
University of Colorado School of Medicine;
Program Co-Leader, Cancer Prevention and Control,
Co-Director, Population Health Shared Resource,
Member, Thoracic Oncology Research Initiative,
University of Colorado Cancer Center
Charles Thomas, MD
Professor and Chief of Radiation Oncology,
Dartmouth-Hitchcock Norris Cotton Cancer Center;
Deputy Editor, JAMA Oncology
Patrecia Valone, MS
Global Head of Clinical Operations, Translational Clinical Oncology,
Novartis Institutes for BioMedical Research (NIBR)
Rev. Gloria E. White-Hammond, MD, MDiv
Co-Pastor, Bethel A.M.E. Church, Boston, MA;
Swartz Resident Practitioner in Ministry Studies,
Harvard Divinity School
Karen Winkfield, MD, PhD
Executive Director, Meharry Vanderbilt Alliance;
Ingram Professor of Cancer Research,
Professor of Radiology Oncology, VUMC;
Professor of Medicine, Meharry Medical College
Robert A. Winn, MD
Director and Lipman Chair in Oncology, VCU Massey Cancer Center;
Senior Associate Dean for Cancer Innovation,
Professor of Pulmonary Disease and Critical Care Medicine,
VCU School of Medicine
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
[value] => ACCOMMODATIONS:
A limited number of rooms have been reserved at the Boston Marriott Cambridge for the nights of April 20 and 21 at nightly rate of $199. Hotel room rates are subject to applicable state and local taxes (currently 14.45% and a 1.5% tourism fee) in effect at the time of check-out. To book your room, you may call Marriott reservations at 1 (800) 228-9290 or (617) 494-6600 and mention the “MGH Cancer Equity Colloquium” room block or CLICK HERE to reserve online. The reservation deadline is Thursday, March 30, 2023.
[format] => full_html
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Recognize and understand existing inequities in cancer care.
- Discuss solutions amongst the treatment team to address factors leading to cancer inequity.
- Develop collaborative initiatives to promote equity in cancer care.
ACCOMMODATIONS:
A limited number of rooms have been reserved at the Boston Marriott Cambridge for the nights of April 20 and 21 at nightly rate of $199. Hotel room rates are subject to applicable state and local taxes (currently 14.45% and a 1.5% tourism fee) in effect at the time of check-out. To book your room, you may call Marriott reservations at 1 (800) 228-9290 or (617) 494-6600 and mention the “MGH Cancer Equity Colloquium” room block or CLICK HERE to reserve online. The reservation deadline is Thursday, March 30, 2023.
For exhibit space, please contact ebrooks3@mgh.harvard.edu
[format] => full_html
)
[field_program] => Array
(
[value] => Friday, April 21, 2023 | 7:15am - 5:30pm
| 7:15am | Registration and Breakfast* |
| 8:00 | Introduction | Colin D. Weekes, MD, PhD & Brenda Lormil, MSN, FNP-C |
| 8:10 | Keynote Address: Improving Cancer Equity through Precision Medicine | Karen Winkfield, MD, PhD |
| 8:55 | Sustained Mentorship: An Integral Component to Achieve Cancer Equity | Charles Thomas, MD |
| 9:25 | Diversity, Inclusion and Equity as Collective Competitive Advantage | Clifton David Fuller, MD, PhD |
| 10:10 | BREAK* |
| 10:25 | Importance of Early Mentorship for Minorities Pursuing Medicine | Kenley Preval |
| 10:45 | Mentorship: Supporting the Growth of the Next Generation | Moderator: Charles Thomas, MD Panelists: Cesar Castro, MD; Kenley Preval; Clifton David Fuller, MD, PhD |
| 11:45am | LUNCH* |
| 12:45pm | Prostate Cancer Community Engagement and the Male Patient | Jean Claude Noel, MS, MA |
| 1:05 | The Compounding Effects of Cancer: "My Voice, My Story, My Truth" Moderator: Brenda Lormil, MSN, FNP-C Panelists: Crystal Davis, RN; Mike Moise, MSA, CPA; Stanley Rameau; Taneshia Camillo-Sheffey |
| 2:05 | Improved Survival in Cancer but Continued Disparities: Planning the Future with Precision Medicine, but Assessing the Past through the Rear View Mirror | Edith Mitchell, MD |
| 2:35 | BREAK* |
| 2:50 | How Can I Help You? Navigating Barriers to Care | Moderator: Brenda Lormil, MSN, FNP-C Panelists: Michelle Barber, MS, GNP-BC, AOCNP; S. Autumn Gaston, BSN, RN; Nora Hathaway, NP; Natasha Gross Jean, RN, BSN, OCN |
| 3:50 | Democratization of Technology | Cesar Castro, MD |
| 4:35 | Overcoming Barriers to Representative Clinical Trial Enrollment | Jamie L. Studts, PhD |
| 5:20 | Closing Remarks |
| 5:30pm | Adjourn |
7:00pm – Welcome Reception @ Artists for Humanity (100 West 2nd Street, Boston, MA 02127)
Complimentary transportation will be provided from meeting venue
*The exhibit hall will be open during breakfast, breaks, and lunch
Saturday, April 22, 2023 | 7:15am - 4:00pm
| 7:15am | Breakfast* |
| 8:00 | Welcome | Colin D. Weekes, MD, PhD & Brenda Lormil, MSN, FNP-C |
| 8:05 | The Role of Cancer Centers in Community Engagement | Moderator: Colin D. Weekes, MD, PhD Panelists: A. William Blackstock Jr., MD; Ruben A. Mesa, MD, FACP; Robert A. Winn, MD |
| 9:05 | Faith-Based Leadership, Support, and Advocacy Panel | Moderator: Karen Burns White Panelists: Cesar Depaz; Rev. Deborah Hamilton, MDiv, BSN, RN, FCN; Rev. Jean J.M. Louis; Rev. Gloria E. White-Hammond, MD, MDiv |
| 10:05 | BREAK* |
| 10:20 | Inequities in Cancer Health Outcomes: Can Strategies Leveraging Noncoding RNA Biology Helps? | Olorunseun (Seun) Ogunwobi, MD, PhD |
| 11:05 | Pharmaceutical Industry Initiatives to Approach Cancer Inequity | Panelists: Neelima Denduluri, MD, FASCO, Lisa Lewis, MPH; Megan McKenzie, MA; Patrecia Valone, MS |
| 12:05pm | LUNCH* |
| 12:50 | Using Healthcare Delivery Systems to Improve Cancer Health Equity | Christopher Lathan, MD, MS, MPH |
| 1:35 | Community-Based Research to Understanding Lung Cancer | Raymond Osarogiagbon, MD, FACP |
| 2:20 | Cancer Equity Programs in Rural America | Electra A. Paskett, PhD |
| 3:05 | BREAK* |
| 3:20 | Fireside Chat | Karen Winkfield, MD, PhD & Colin Weekes, MD, PhD |
| 4:05pm | Adjourn |
*The exhibit hall will be open during breakfast, breaks, and lunch
NON-HEALTHCARE PROFESSSIONALS
CLICK HERE for free registration
Professionals from healthcare and related industries must pay the registration fee to receive continuing education (CE) credit.
Cancellation Policy:
Registrations cancelled on or before April 7, 2023 will be refunded, less a $15 administrative fee. Registrations cancelled after April 7, 2023 will not be refunded.
Contact partnerscpd@partners.org if you require assistance in cancelling your online registration.
ACCOMMODATIONS:
A limited number of rooms have been reserved at the Boston Marriott Cambridge for the nights of April 20 and 21 at nightly rate of $199. Hotel room rates are subject to applicable state and local taxes (currently 14.45% and a 1.5% tourism fee) in effect at the time of check-out. To book your room, you may call Marriott reservations at 1 (800) 228-9290 or (617) 494-6600 and mention the “MGH Cancer Equity Colloquium” room block or CLICK HERE to reserve online. The reservation deadline is Thursday, March 30, 2023.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for Physicians, Nurses, Pharmacists, Psychologists, Physician Assistants, Social Workers, Other members of the healthcare team, General Public, and Patients & Caregivers.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/2466 [id] => 2466 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital Cancer Center & Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=69216
[first] => https://cpd.partners.org/node?nid=69216&page=0
[last] => https://cpd.partners.org/node?nid=69216&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statement
AMA PRA Category 1 Credits™
Mass General Brigham designates this live activity for a maximum of 6 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1704722400
[value2] => 1711771140
[duration] => 7048740
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1709211600
[value2] => 1709236800
[duration] => 25200
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/7
[id] => 7
[resource] => taxonomy_term
[uuid] => 2a38b69f-4c76-44b0-bde5-67e901205c53
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/61149
[id] => 61149
[resource] => file
[uuid] => 2ea8cbc0-3ebe-4ae4-88b6-7baf0b0556bc
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 48585
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Livestream via Massachusetts General Hospital
[street] => 55 Fruit Street
[additional] =>
[city] => Boston
[province] => MA
[postal_code] => 02114
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => 
This conference is free of charge thanks to the support of the American Institute for Neuro Integrative Development (AIND), the Genesis Foundation for Children
THIS IS A VIRTUAL COURSE
You will receive the Zoom link upon registering.
More than 10,000 rare diseases are estimated to impact over 30 million Americans. Unfortunately, many individuals remain undiagnosed, leading to prolonged and challenging journeys in pursuit of understanding and proper care. These often place significant burdens on families and strain our medical system. Rapid advancements in genetics have significantly enhanced our diagnostic capabilities and care recommendations, with targeted therapies emerging for select disorders. However, navigating the complex landscape of evaluation and testing options for diagnosis remains a challenge for both families and medical professionals. This program is designed to provide patients, families, and healthcare providers (including both primary and specialty physicians) with the latest insights into a genetic evaluation. Featuring six expert MGH/HMS genetics providers and families of patients, the course covers clinically relevant fundamentals of human genetics, genetic counseling, and the latest technological advancements in diagnostics and therapies.Through engaging lectures and real-life patient perspectives, participants will enhance their understanding of the intricacies surrounding rare genetic disorders. Whether you are a family facing the challenges of diagnosis, a medical provider, or someone with a general interest in the field, this program aims to empower attendees with knowledge to advocate for those affected by these unique conditions.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => David Sweetser, MD, PhD - Course Director
Clinical Geneticist, Research Scientist,
Chief of Medical Genetics and Metabolism,
MGH Site Director Undiagnosed Diseases Network,
Co-Director Pitt Hopkins Clinic,
Massachusetts General Hospital
Frances High, MD, PhD
Clinical Geneticist, Research Scientist, Co-Director Klinefelter Syndrome Clinic,
Director of Reproductive Endocrinology and Infertility Genetics, Massachusetts General Hospital for Children
Angela Lin, MD
Clinical Geneticist, Co-Director Turner Syndrome and Myhre Syndrome Clinics,
Director Pediatric Hereditary Hemorrhagic Telangiectasia Center, MassGeneral for Children
Catherine Nowak, MD
Clinical Geneticist, Clinical Director, Division of Medical Genetics and Metabolism,
Massachusetts General Hospital for Children
Melissa Walker, MD, PhD
Neurologist, Research Scientist, Director Neuro-Pediatric Mitochondrial Disorders Clinic,
Massachusetts General Hospital for Children
Ashley Wong, MS, LCGC
Genetic Counselor, Massachusetts General Hospital for Children
Assistant Professor, MGH Institute of Health Professions
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Recognize the value as well as strengths, limitations, and pitfalls of genetic testing.
- Identify the common diagnostic genetic tests used and gain familiarity with test result interpretation.
- Recognize the value of multidisciplinary coordinated care for individuals with rare genetic syndromes.
- Recognize genetic disorders currently amenable to targeted therapies and new therapeutic possibilities on the horizon.
ABP MOC RECOGNITION STATEMENT
Successful completion of this CME activity, which includes participation in the evaluation component, enables the learner to earn up to 6 MOC points in the American Board of Pediatrics’ (ABP) Maintenance of Certification (MOC) program. It is the CME activity provider’s responsibility to submit learner completion information to ACCME for the purpose of granting ABP MOC credit.
ABIM MOC RECOGNITION STATEMENT
Successful completion of this CME activity, which includes participation in the activity, with individual assessments of the participant and feedback to the participant, enables the participant to earn 6 MOC points in the American Board of Internal Medicine (ABIM) Maintenance of Certification (MOC) program. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
[format] => full_html
)
[field_program] => Array
(
[value] => | 8:00am | Welcome Remarks | David Sweetser, MD, PhD |
| 8:15 | Embarking on the journey: “Could there be a genetic cause?" | Catherine Nowak, MD |
| 9:00 | Complexities of interpreting genetic test results: “This test report is confusing, what does it mean?” | Ashley Wong, MS CGC |
| 9:45 | BREAK |
| 10:00 | Our test result indicates there may be a diagnosis. “Now what”? | Frances High, MD, PhD |
| 10:45 | At the end of the diagnostic odyssey: Seeking a home for coordinated care. "Where, Who, How?" | Angela Lin, MD |
| 11:30 | Parent Perspective Panel | Matthew Hoffman, Jessica Fieber, Zhanna Ullman |
| 12:30pm | LUNCH BREAK |
| 1:00 | What's on the horizon for diagnostic genetic testing? | David Sweetser, MD, PhD |
| 1:45 | What’s on the Horizon for Targeted Therapies? | Melissa Walker, MD PhD |
| 2:30 | Speaker Panel Discussion | David Sweetser, MD, PhD; Catherine Nowak, MD; Ashley Wong, MS CGC; Frances High, MD, PhD; Angela Lin, MD; Melissa Walker, MD PhD |
| 3:00pm | Farewell/Adjourn |
[format] => full_html ) [field_registration_instructions] => Array ( ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>
This activity is intended for Physicians, Nurses, Nurse Practitioners, Dentists, Dieticians, Psychologists, Physician Assistants, and Social Workers across the country, as well as General Public, and Patients & Caregivers.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3103 [id] => 3103 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital and Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=70302
[first] => https://cpd.partners.org/node?nid=70302&page=0
[last] => https://cpd.partners.org/node?nid=70302&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this live activity for a maximum of 16.75 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 16.75 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1711127160
[value2] => 1729569540
[duration] => 18442380
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1725796800
[value2] => 1726000200
[duration] => 203400
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/238
[id] => 238
[resource] => taxonomy_term
[uuid] => fd81c17a-d19b-46b8-ad6b-2c5aee9ce9be
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/65503
[id] => 65503
[resource] => file
[uuid] => a475a4a5-f27e-4cd5-b54d-91cbc54bc5b3
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 50671
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Fairmont Copley Plaza
[street] => 138 St James Ave.
[additional] =>
[city] => Boston
[province] => MA
[postal_code] => 02116
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => Current treatment strategies for patients with complex digestive disorders continue to evolve. This is largely the result of growing technological advances in surgery and endoscopy. The goal of the Minimally Invasive and Novel Therapeutics (MINT) course is to inform physicians on how best to incorporate these technologies into their practice. Using a video-based format, our goal is technique transfer from world-renowned faculty to the community, hospital, endoscopy suite, and operating room. MINT offers an ideal mix of traditional standard-of-care principles with a balanced and unbiased view of new, cutting-edge information. This hybrid course (in-person and virtual) engages learners through video-based lectures with recordings of surgical and endoluminal therapies, along with lively multidisciplinary panel discussions.
Digestive disease management requires multidisciplinary care. This course intends to break the barriers of subspecialty medicine by bringing together gastroenterologists, surgeons, psychologists, APPs, nurses, and dietitians to learn from each other. Since many surgeons and endoscopists learn best by “doing”, this course offers hands-on skills sessions in both endoluminal therapies and surgical techniques taught by national and international experts.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Course Directors
Charu Paranjape, MBBS
Faculty at Harvard Medical School
Program Director, Robotic Education,
Massachusetts General Hospital
Associate Chair and Chief of General Surgery
Mass General Brigham,
Newton-Wellesley Hospital
Kumar Krishnan, MD
Assistant professor of Medicine,
Harvard Medical School;
Director of Endoscopic Innovation, Technology and Education,
Massachusetts General Hospital
Hany Takla, MD, FACS, FASMBS, DABS-FPMBS
General & Bariatric Surgeon
Medical Director of Surgical services
Chair Department of Surgery
General Surgery Dover I Center for Weight Management and Bariatric Surgery
Wentworth Douglass Hospital
Massachusetts General Hospital
Faculty
Abdelrahman Nimeri, MD, FACS
Gastrointestinal and General Surgery,
Director of Bariatric Surgery, Brigham and Women’s Hospital
Adham Saad, MD, FACS
Assistant Professor, Surgery
Fellow, Minimally Invasive Surgery
University of South Florida Health
Alexandra Maltby, PA-C
General Surgery Physician Assistant,
Department of Surgery,
Newton-Wellesley Hospital
Ali Tavakkoli, MD
Associate Professor, Harvard Medical School;
Chief, Division of General and GI Surgery,
Co-Director, Center for Weight Management and Wellness,
Program Director, Advanced Minimally Invasive Fellowship,
Brigham and Women’s Hospital
Aman Ali, MD
Bariatric Surgery, General Surgery,
Department of Surgery, Houston Methodist
Ankit Patel, MD
General and Bariatric surgeon,
Associate professor of Surgery
Emory University
Annaliessa Visco, RD
Ashraf Maghrabi, MD, FRCSC
President, Saudi General Surgery Society
Associate Professor of Surgery
Thoracic, Foregut and Bariatric Surgeon
King Abdulaziz University Hospital
Ashvind Bawa, MS, FACS
Professor Surgery
Dayanand Medical College and Hospital
Ludhiana, Punjab, India
Ashwin Ananthakrishnan, MBBS, MPH
Gastroenterologist,
Massachusetts General Hospital
Brittany Mallette, RN
B. Ramana, MBSS, MS, FRCS, FACS, FIBC, FISA
General and hernia surgery
Goulburn Valley Health, Shepparton, Victoria, Australia
Founder and President of AWR Surgeons Community
Dana Telem, MD
Section Head of General Surgery,
Associate Chair for Quality and Patient Safety,
Lazar J. Greenfield Professor of Surgery,
University of Michigan Health
David Lourié, MD
Director of MIS program at Huntington Hospital
Deepak Subramanian, MD
Clinical Lead, Dept of Laparoscopic and Bariatric Surgery
MGM HEALTHCARE, Chennai
Denise Gee, MD
Bariatric Surgeon
Vice Chair of Clinical Operations, Department of Surgery,
Surgical Director, Mass General Weight Center,
Section Head, Swallowing,
Heartburn and Esophageal Disease Program, Massachusetts General Hospital
Elan Witkowski, MD, MS
Gastrointestinal Surgeon,
Head, Hernia Center,
Massachusetts General Hospital
Emily Letendre, PA-C
Department of Surgery,
Newton-Wellesley Hospital
Eran Brauner, MD
General Surgery, Newton-Wellesley Hospital
Eric Pauli, MD, FACS, FASGE
David L. Nahrwold Professor of Surgery
Chief, Division of Minimally Invasive and Bariatric Surgery
Vice Chair, Clinical Affairs
Director of Abdominal Wall Surgery
Program Director, Abdominal Wall Surgery Fellowship
Department of Surgery
Penn State Health
Firas El-Hanafi, MD, FACS, FRCSEd(Gen. Surg), FRCSEd(OG)
Senior Upper GI and Bariatric Surgeon,
Darlington Memorial Hospital;
County Durham and Darlington NHS
Foundation Trust,
United Kingdom
George Velmahos, MD, PhD
John F. Burke Professor of Surgery, Harvard Medical School;
Division Chief of Trauma, Emergency Surgery and Surgical Critical Care,
Massachusetts General Hospital
Hassan Mashbari, MD
Assistant professor in Surgery,
General Surgery Residency Program Director,
Director, Clinical Simulation & Life Support Center,
Jazan University
Jignesh Gandhi, MD
Senior Consultant,
Robotic, GI & Laparoscopic Surgeon,
Gleneagles Hospital | Mumbai
Jennifer Lopes, RN
Endoscopy Registered Nurse,
Newton-Wellesley Hospital
John DeWitt, MD
Professor of Medicine,
Director of Endoscopic Ultrasound,
Indiana University Health
John Pandolfino, MD
Chief of Gastroenterology and Hepatology in the Department of Medicine,
Hans Popper Professor,
Professor of Medicine (Gastroenterology and Hepatology),
Northwestern University Feinberg School of Medicine
Kathryn Schlosser, MD
General Surgery, Beth Israel Deaconess Medical Center
Laura Shannon, RN
Lee Kaplan, MD, PhD
Professor of Medicine,
Dartmouth Geisel School of Medicine
Mario Gonçalves
Abdominal wall surgeon
Fellow of the European Board of Surgery - Abdominal Wall
Fellow of the American College of Surgeons
Hospital de Braga
Braga, Portugal
Matthew Hutter, MD, MPH, MBA
Professor in Surgery, Harvard Medical School;
Gastrointestinal Surgeon | Bariatric Surgeon | Laparoscopic/Minimally Invasive Surgeon
Director of the Codman Center for Clinical Effectiveness in Surgery,
Massachusetts General Hospital
Michael DeWane, MD
General Surgery, Massachusetts General Hospital
Mohit Bhandari, MS, DMAS, FICS, FIAGES, FALS
Director Mohak Bariatrics and Robotics, Indore, India
Nari Sabeti, MD
General and Gastrointestinal Surgery, Weight Loss (Bariatric) Surgery
Medical Director, Surgical Weight Loss Program
Salem Hospital
Nora Fullington, MD
Partner, Boston Hernia
Newton-Wellesley Hospital
Omar Ghanem, MD
Chair, Division of Metabolic and abdominal wall reconstructive surgery
Associate professor of Surgery
Mayo Clinic, Rochester, MN
Pawanindra Lal, MD
Department of Surgery,
Maulana Azad Medical College
Peter Fagenholz, MD
Associate Professor of Surgery, Harvard Medical School;
Pancreatic and General Surgeon,
Surgical Director, MGH Pancreatitis Treatment Center,
Massachusetts General Hospital
Pramod Shinde, MD
Bariatric Surgeon, General Surgeon, Laparoscopic Surgeon,
Kaushalya Hospital & Research Centre | Nashik
Prakash Gatta, MD
Texas Christian University, Brunette School of Medicine,
Fort Worth, TX
Premkumar Balachandran, MD
Clinical Lead, Apollo Institutes of Hernia Surgery and Abdominal Wall Reconstruction
Apollo Hospitals
Priyanca Waghmarae, PA-C
Outpatient Gastroenterology, Massachusetts General Hospital
Rahul Mahadar, MD
Senior Gastrointestinal Surgeon,
Jeevanshree Hospital
Rajesh Shrivastava, MD
Bariatric & Laparoscopic Surgeon
Ralph Weissleder, MD, PhD
Thrall Family Professor of Radiology,
Professor of Systems Biology,
Harvard Medical School;
Center for Systems Biology,
Radiologist, Interventional Radiology,
Massachusetts General Hospital
Rana Pullat, MD, FACS, FASMBS
Professor of Surgery,
Director of Bariatrics and Robotic Surgery
Division Chief of Foregut and Metabolic Surgery,
Medical University of South Carolina
Reem Sharaiha, MD, MSc
Gastroenterology, Weill Cornell Medicine
Rocco Ricciardi, MD
Colorectal Surgeon | Gastrointestinal Surgeon
Chief, Section of Colon and Rectal Surgery,
Massachusetts General Hospital
Roy Patankar, MD
Director and Administrative Head,
Zen Multispeciality Hospital
Sanjay Sonar, MD
General Surgeon, Godrej Memorial Hospital | Mumbai
Sharad Sharma, MD
Bariatric Surgeon, Fortis Hospital Mulund | Mumbai
Sheila Partridge, MD
General Surgery, Bariatric Surgery,
Newton-Wellesley Hospital
Suha K. Kaaki, MD, FRCSC FACS
Assistant Professor of Surgery
Program Director, Thoracic Surgery Fellowship Thoracic and Foregut Surgeon
King Saud University Medical City
Susana Wishnia, MD
General Surgery, Bariatric Surgery,
Newton-Wellesley Hospital
Uzma Siddiqui, MD
Professor of Medicine
Director, Endoscopic Ultrasound and Advanced Endoscopy Training
Director, Center for Endoscopic Research & Therapeutics
University of Chicago Medicine
Vivek Bindal, MD
Director & Head,
Max Institute of Minimal Access, Bariatric & Robotic Surgery
Yalini Vigneswaran, MD
Advanced GI and Bariatric Surgery
Surgical Director of Education Institute
Program Director of Esophageal Diseases
University of Chicago Medicine
Yusef Kudsi, MD, MBA, FACS,
Gastrointestinal and General Surgery,
Brigham and Women’s Hospital
Shannon Gagnon, RN
Operating room RN
MGB-Wentworth Douglass Hospital
Christina Warne, DPT, PT
Rehabilitation and physical therapy
MGB-Wentworth Douglass Hospital
Kendal Towle, APRN
General and Bariatric surgery
MGB-Wentworth Douglass Hospital
Ramesh Punjani, MS, FACS, FICS, FMAS, FIAGES
General, Laparoscopic & Robotic Surgeon,
Special Interest: Hernia & Abdominal Wall Reconstruction,
Director: Pooja Nursing Home Pvt. Ltd.
Senior Surgeon: Fortis Hospital, Mulund
Visiting Surgeon: Jupiter Hospital; Breach Candy Hospital; P D Hinduja National Hospital, Mahim
Director: Master Hernia Course, IMMAST, Worli, Mumbai
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
[value] => NOTE: Sunday 9/8 will be held at a different location, TBD
[format] => full_html
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Apply new knowledge in the management of patients with foregut disease, abdominal wall hernias, and pancreaticobiliary disease.
- Develop treatment strategies based on current evidence and expert opinion.
- Compare and contrast standard-of-care management with cutting-edge treatments.
- Recognize the unique roles and contributions of various healthcare professionals within the multidisciplinary foregut team.
- Collaborate effectively among multidisciplinary team members to improve patient outcomes.
Maintenance of Certification (MOC)
American Board of Surgery (ABS) MOC Recognition Statement
Successful completion of this CME activity, which includes participation in the evaluation component, enables the learner to earn credit toward the CME requirement of the American Board of Surgery’s Continuous Certification program. It is the CME activity provider's responsibility to submit learner completion information to ACCME for the purpose of granting ABS credit.
American Board of Internal Medicine (ABIM) MOC Recognition Statement
Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to 16.75 MOC point in the American Board of Internal Medicine’s (ABIM) Maintenance of Certification (MOC) program. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
[format] => full_html
)
[field_program] => Array
(
[value] => *Agendas are subject to change*
Sunday, September 8, 2024 | NO CREDIT
7:00 am | Introduction to course & Welcome |
7:15 | Resident/Fellow robotic hands-on sessions | |
12:00 pm | Lunch |
Resident Didactic Session | |
1:00 | Back to Basics Anatomy Session | David Lourié |
1:30 | How to Build a Practice and Get Referrals | Susana Wishnia |
1:50 | Q&A |
2:00 | Negotiation Skills | Aman Ali |
2:20 | Simulation and Synthetic Models in Surgical Education | Mario Gonçalves |
2:30 | How to Handle Complications | Eric Pauli |
2:50 | Q&A |
3:00 | Robotic Surgeon: A marketing tool or a real edge? | Ankit Patel |
| 3:30 | Technique Transfer: Tips and Tricks | Rahul Mahadar; Pawanindra Lal; Prakash Gatta |
4:15 | MINT Video Abstract Competition |
5:00 pm | Adjournment of Resident Didactic Session |
Attending Hands on Robotic Surgery Session Panelists/Faculty: Suha Kaaki; Ankit Patel; Aman Ali; Susana Wishnia; Eran Brauner; Prakash Gatta; Mario Gonçalves; Firas El-Hanafi, MD, FACS, FRCSEd(Gen. Surg), FRCSEd(OG) | |
Monday, September 9, 2024
| 8:00am | Introduction to Course & Welcome | Charu Paranjape & Kumar Krishnan |
The Complex Esophageal Patient | |
8:15 | Persistent Dysphagia | Panelists: Dana Telem; John Pandolfino; Elan Witkowski; Kumar Krishnan; Charu Paranjape |
8:45 | Role and Choice of Antireflux Surgery in Patients with Barrett’s Esophagus | Panelists: John Pandolfino; Elan Witkowski; Kumar Krishnan; Charu Paranjape; Suha K. Kaaki |
9:05 | Complex POEM: Tips and Tricks | Panelists: Kumar Krishnan; Elan Witkowski; Uzma Siddiqui; Reem Sharaiha |
9:25 | Keynote Address: EndoFLIP in 2024- What the Practicing Endoscopist and Surgeon Needs to Know | John Pandolfino |
9:55 | BREAK |
Innovative Strategies to Manage Foregut Disease | |
10:05 | Management of Foregut Leak and Fistula | Panelists: Eric Pauli; Ali Tavakkoli; John Pandolfino; Reem Sharaiha |
10:25 | Remote Robotic Platforms | Panelists: Denise Gee; Yalini Vigneswaran; Roy Patankar |
10:45 | From Novice to Expert: Improving your skillset in POEM | Speaker: Kumar Krishnan Panelists: Eric Pauli; John DeWitt; Uzma Siddiqui; Reem Sharaiha |
11:05 | PORSHA Flap | Panelists: Charu Paranjape; Yusef Kudsi; Dana Telem |
11:35 | Redo Redo Redo vs Redo Redo Bypass | Panelists: Eric Pauli; Ali Tavakkoli; Charu Paranjape; Kumar Krishnan; Uzma Siddiqui; Reem Sharaiha |
11:55 | Keynote Address: Bringing Law and Order to the Wild West | Dana Telem |
12:25pm | Wrap up and Questions |
12:30pm | LUNCH BREAK |
| 1:30 | Endoluminal Hands-on Session (rotating stations) Station 1: ESD | Uzma Siddiqui |
APP/RN Session: MINT Multidisiplinary Team | |
| 1:30 | Complex Esophageal Case/Barrett's Esophagus | Adham Saad; Jennifer Lopes-DeCarvalho; Priyanca Waghmarae; Laura Shannon, Brittany Mallette |
| 2:00 | Complex Biliary Case | Hany Takla; Kendal Towle; Priyanca Waghmarae; Laura Shannon, Brittany Mallette |
| 2:30 | OR Efficiency | Shannon Gagnon & Pawan Lal |
| 3:00 | BREAK |
| 3:10 | Complex Bariatric Case | Rana Pullatt; Kendal Towle; Nari Sabeti; Annaliessa Visco, RD |
| 3:40 | Complex Hernia Case | Yusef Kudsi; Christina Warne; Emily Letendre |
| 4:10 | Wrap up and questions |
| 4:15pm | Adjourn |
Tuesday, September 10, 2024
MINT BariatricPanelists: Denise Gee; Ali Tavakkoli; Sheila Partridge; Reem Sharaiha; Abdelrahman Nimeri; Hany Takla | |
| 8:00am | Weight regain after RYGB: options and challenges | Abdelrahman Nimeri |
| 8:20 | Surgical management of sleeve fistula and chronic complications after bariatric surgery | Rana Pullatt |
| 8:40 | Revisional Bariatric Surgery: When/ How/ Why? | Omar Ghanem |
| 9:00 | Novel Innovations in Bariatric Surgery | Mohit Bhandari |
| 9:20 | Novel Innovations in Bariatric Endoscopy | Reem Sharaiha |
| 9:40 | Pharmacotherapy For Weight Loss in 2024 and Beyond | Lee Kaplan |
| 10:00 | LINX after Bariatric Surgery | Ashraf Maghrabi |
| 10:15 | BREAK |
MINT Multidisciplinary Management: PancreaticobiliaryPanelists: John DeWitt, Uzma Siddiqui, Kumar Krishnan, Reem Sharaiha, Charu Paranjape | |
| 10:25 | Stones in the Postoperative Patient | Uzma Siddiqui |
| 10:45 | EUS Biliary Drainage: How To | John DeWitt |
| 11:05 | All in One Approach: Lap CBDE to the Rescue? | Eric Pauli |
| 11:25 | Percutaneous Management of Strictures and Stones | Ralph Weisslader |
| 11:45 | Multidisciplinary Management of Complex Pancreatitis | Peter Fagenholz |
| 12:15pm | LUNCH |
MINT Hernia and Abdominal WallCo-Directors: Hany Takla & Elan Witkowski | |
| 12:45 | Know Your Anatomy for the Attending Surgeon | Panelists: Matthew Hutter; Dana Telem; B. Ramana; Nora Fullington; Ramesh Punjani |
| 1:05 | New Robotic Platforms: Comparisons, Advantages, and Challenges | |
| 1:20 | How to Navigate Complex Hernia as a New Attending? | Speaker: Kathryn Schlosser Panelists: Matthew Hutter; Dana Telem; B. Ramana; Nora Fullington; Ramesh Punjani |
| 1:35 | AWR in 2024: What’s out there to know? Speaker: Yusef Kudsi Panelists: Matthew Hutter; Dana Telem; B. Ramana; Nora Fullington; Ramesh Punjani |
| 1:50 | E-TEP Inguinal Hernia Repair - Troubleshooting Speaker: Jignesh Gandhi Panelists: Matthew Hutter; Dana Telem; B. Ramana; Nora Fullington; Ramesh Punjani |
| 2:05 | Abdominal Fistula in the IBD Patient | Speakers: Ashwin Ananthakrishnan & Rocco Ricciardi Panelists: Matthew Hutter; Dana Telem; B. Ramana; Nora Fullington; Ramesh Punjani |
| 2:25 | Measuring Individual Performance and Quality Data to Better Your Hernia Practice | Speaker: Yalini Vigneswaran Panelists: Matthew Hutter; Dana Telem; B. Ramana; Nora Fullington; Ramesh Punjani |
| 2:35 | TAR gone wrong; can I fix it? | Speaker: Michael DeWane Panelists: Matthew Hutter; Dana Telem; B. Ramana; Nora Fullington |
| 2:50 | Lateral Hernias: Ten Things You Should Know | |
| 3:00 | Surgeon’s Edge: AI Tool for the Modern Surgeon | |
| 3:10 | BREAK |
| MINT Hernia | |
| 3:20 | Weight loss and AWR: too idealistic? | Speaker: Sharad Sharma Panelists: George Velmahos; Nari Sabeti; Pramod Shinde |
| 3:30 | Eliminating chronic pain after inguinal hernia surgery | Speaker: Nora Fullington Panelists: George Velmahos; Nari Sabeti; Pramod Shinde |
| 3:45 | Mesh Infections: Does Experience Match with Evidence? | Speaker: Deepak Subramanian Panelists: George Velmahos; Nari Sabeti; Pramod Shinde |
| 3:55 | The abdominal catastrophe | Speaker: B. Ramana Panelists: George Velmahos; Nari Sabeti; Pramod Shinde |
| 4:10 | RIF Hernias: Many Ways to Skin It | Speaker: Sanjay Sonar Panelists: George Velmahos; Nari Sabeti; Pramod Shinde |
| 4:20 | Hernia centers of excellence: a marketing gimmick or useful quality initiative? | Speaker: Elan Witkowski Panelists: George Velmahos; Nari Sabeti; Pramod Shinde |
| 4:30 | Parastomal Hernias: A Short Ride | Speaker: Premkumar Balachandran Panelists: George Velmahos; Nari Sabeti; Pramod Shinde |
| 4:40 | The most useful tools for the MIS hernia surgeon | Speaker: Rahul Mahadar Panelists: George Velmahos; Nari Sabeti; Pramod Shinde |
| 4:50 | Post liver transplant hernias: surgical considerations | Speaker: Rajesh Shrivastava Panelists: George Velmahos; Nari Sabeti; Pramod Shinde |
| 5:00pm | Adjourn |
[format] => full_html ) [field_registration_instructions] => Array ( [value] =>
Physicians | ||
Registration Type | Early Bird Tuition Fees | Regular Tuition Fees |
Didactic MINT course ONLY | $350.00 | $400.00 |
Didactic MINT course AND Hands-On Endoluminal (Monday 9/9) | $550.00 | $600.00 |
Didactic MINT course AND Hands-On Robotics HANDS-ON ROBOTICS SESSION FULL | $1,050. 00 | $1,100.00 |
Hands-On Robotics (Sunday 9/8) | $1,250.00 | $1,300.00 |
International Physicians - Didactic MINT course ONLY | N/A | $250.00 |
International Physicians - Didactic MINT course AND Hands-On Robotics (Sunday 9/8) HANDS-ON ROBOTICS SESSION FULL | N/A | $950.00 |
| International Physicians - Didactic MINT AND Hands-On Endoluminal (Monday 9/9) | N/A | $450.00 |
| International Physicians Hands-On Robotics (Sunday 9/8) Hands-On Endoluminal (Monday 9/9) Didactic MINT course (Monday 9/9 & Tuesday 9/10) | N/A | $1,400.00 |
United States Residents & Fellows | ||
Registration Type | Early Bird Tuition Fees | Regular Tuition Fees |
Didactic MINT course ONLY | N/A | $75.00 |
Didactic MINT course AND Hands-On Endoluminal | N/A | $75.00 |
REGISTRATION FULLResident Didactic Session & Hands-On Robotics | N/A | $75.00 |
REGISTRATION FULLResidents - | N/A | $75.00 |
REGISTRATION FULLResidents - | N/A | $75.00 |
Nurses, APPs, & Allied Health Professionals | ||
Registration Type | Early Bird Tuition Fees | Regular Tuition Fees |
Didactic MINT course ONLY | $100.00 | $150.00 |
Industry | ||
Registration Type | Early Bird Tuition Fees | Regular Tuition Fees |
Didactic MINT course ONLY | N/A | $400.00 |
Cancellation Policy:
Registrations cancelled on or before August 26, 2024 will be refunded, less a $50 administrative fee. Registrations cancelled after August 26, 2024 will not be refunded.
Contact partnerscpd@partners.org if you require assistance in cancelling your online registration.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for Physicians, Nurses, Nurse Practitioners, Dieticians, Physician Assistants, and other members of the healthcare team.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3183 [id] => 3183 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Newton-Wellesley Hospital, Massachusetts General Hospital, and Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=68062
[first] => https://cpd.partners.org/node?nid=68062&page=0
[last] => https://cpd.partners.org/node?nid=68062&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this live activity for a maximum of 9.50 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 9.50 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
Physician Assistants
Mass General Brigham has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 9.50 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation.

ABA MOC Statement
This activity contributes to the CME component of the American Board of Anesthesiology’s redesigned Maintenance of Certification in AnesthesiologyTM (MOCA®) program, known as MOCA 2.0®. Please consult the ABA website, www.theABA.org, for a list of all MOCA 2.0 requirements.
ABS MOC Statement
Successful completion of this CME activity, which includes participation in the evaluation component, enables the learner to earn credit toward the CME requirement of the American Board of Surgery’s Continuous Certification program. It is the CME activity provider's responsibility to submit learner completion information to ACCME for the purpose of granting ABS credit.
ABOHNS MOC Statement
Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn their required annual part II self-assessment credit in the American Board of Otolaryngology – Head and Neck Surgery’s Continuing Certification program (formerly known as MOC). It is the CME activity provider's responsibility to submit participant completion information to ACCME for the purpose.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1698241440
[value2] => 1719806340
[duration] => 21564900
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1710428400
[value2] => 1710534600
[duration] => 106200
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/60191
[id] => 60191
[resource] => file
[uuid] => 7766612e-42c9-4b9f-8809-eac1bd5be78b
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => THIS IS A VIRTUAL COURSE
In the United States, almost 40% of all inpatient procedures are performed on patients aged 65 and older; at MGB trauma centers over 50% of injured patients are older adults, the majority of whom are frail. To prepare our healthcare system to care for growing numbers of older adults who have increasing medical and psychosocial complexity, front line clinicians including Advanced Practice Providers (APPs), surgical trainees, nurses, and surgical attendings urgently need more training in geriatric syndromes and the 5 pillars of Age-Friendly care (Medication, Mobility, what Matters, Mentation and Multicomplexity). This training will address the needs of the growing number of geriatric patients, and avoid hazards of hospitalization such as delirium, falls, infections, and loss of function, and reduce caregiver strain. These issues are particularly relevant in surgery and trauma where mortality, complications, and other adverse outcomes are consistently higher for older patients than their younger counterparts. Moreover, national stakeholders including CMS and the American College of Surgeons are setting standards for geriatric surgical care that clinicians must be prepared to meet. Evidence suggests that geriatric-focused clinical pathways can reduce delirium, ICU stays, length of stay, and readmissions in older surgical patients. Clinicians will benefit from in depth training in geriatric care to enable the implementation of structures and processes to improve outcomes.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Course Directors
Zara Cooper, MD, MSc
Michele and Howard J. Kessler Distinguished Chair of Surgery and Public Health
Kessler Director, Center for Surgery and Public Health
Director, Center for Geriatric Surgery, Brigham and Women’s Hospital
Professor of Surgery, Harvard Medical School
Rachelle Bernacki, MD, MS
Director of Care Transformation and Postoperative Services, Center for Geriatric Surgery, Brigham and Women’s Hospital
Director of Quality Initiatives, Psychosocial Oncology and Palliative Care, Dana Farber Cancer Institute
Associate Professor of Medicine, Harvard Medical School
Julia Loewenthal, MD
Geriatrician, Division of Aging, Brigham and Women’s Hospital
Assistant Program Director, Internal Medicine Residency Program, Brigham and Women’s Hospital
Instructor in Medicine, Harvard Medical School
Andrea Wershof Schwartz, MD, MPH
Geriatrician, Division of Aging, Brigham and Women’s Hospital
Associate Professor of Medicine, Harvard Medical School
Associate Director, New England Geriatric Research Education and Clinical Center, VA Boston Healthcare System
Course Planners
Amy Bulger, RN, MPH, GERO-BC, CPHQ
Director of Geriatrics Operations, Center for Geriatric Surgery and Department of Nursing, Brigham and Women’s Hospital
Lynne O'Mara, MPAS, PA-C
Clinical Program Manager, Center for Geriatric Surgery, Brigham and Women’s Hospital
Senior Administrator of Inpatient Operations, Brigham and Women’s Hospital
Course Speakers
Roman Belenkiy, PharmD, BCGP
Transitions of Care Pharmacist, Brigham and Women’s Hospital
Christy Cauley, MD, MPH
Colorectal and Gastrointestinal Surgeon, Massachusetts General Hospital
Director of Research, MGH Colorectal Surgery
Assistant Professor, Harvard Medical School
Sevdenur Cizginer, MD, MPH, AGSF
Assistant Professor of Medicine, Harvard Medical School
Geriatrician, Massachusetts General Hospital
Stacie Deiner, MD, MS
LeRoy Garth Professor and Vice Chair for Research,
Department of Anesthesiology, Dartmouth Hitchcock Medical Center
Laura Frain, MD, MPH
Geriatrician, Beth Israel Deaconess Medical Center and Brigham and Women’s Hospital
Instructor in Medicine, Harvard Medical School
Esteban Franco Garcia, MD, AGSF
Instructor in Medicine, Harvard Medical School
Program Director, Geriatric Medicine Fellowship, Massachusetts General Hospital
Director, Geriatric Inpatient Fracture and Trauma Service, Massachusetts General Hospital
Tamryn Fowler Gray, PhD, RN, MPH
Clinical Specialist, Department of Medical Oncology, Division of Stem Cell Transplantation and Cellular Therapies
Research Scientist, Phyllis F. Cantor Center for Research in Nursing and Patient Services, Dana-Farber Cancer Institute
Instructor in Medicine, Department of Psychosocial Oncology and Palliative Care, Dana-Farber Cancer Institute, Harvard Medical School
Masaya Higuchi, MD, MPH, CMD, AGSF
Medical Director, MGH Perioperative Optimization of Senior Health Program (POSH)
Division of Palliative Care and Geriatric Medicine, Massachusetts General Hospital
Instructor in Medicine, Harvard Medical School
Houman Javedan, MD
Clinical Director, Division of Aging, Brigham and Women’s Hospital
Assistant Professor of Medicine, Harvard Medical School
Nancy Latham, PhD, PT
Clinical Research Director, Research Division of Men’s Health, Aging and Metabolism, Brigham and Women’s Hospital
Lecturer in Medicine, Harvard Medical School
Deborah Lee, MD
Geriatrician, Massachusetts General Hospital
Instructor in Medicine, Harvard Medical School
Sharon Levine, MD
Section Head, Geriatric Medicine, Division of Palliative Care and Geriatric Medicine, Massachusetts General Hospital
Professor of Medicine, Director of Geriatrics Education Innovation, Boston University School of Medicine
Elizabeth Lilley, MD, MPH
Surgical Oncologist, Brigham and Women’s Hospital
Affiliate Faculty, Department of Psychosocial Oncology and Palliative Care, Dana-Farber Cancer Institute
Associate Program Director, Mass General Brigham/Dana-Farber Complex General Surgical Oncology Fellowship, Harvard Medical School
Ariela Orkaby, MD, MPH
Geriatrician, Director of Frailty Research, Division of Aging, Brigham and Women’s Hospital
Associate Director for Research Training, New England Geriatric Research Education and Clinical Center, VA Boston Healthcare System
Assistant Professor of Medicine, Harvard Medical School
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Describe the 5 Ms (Medication, Mobility, what Matters, Mentation, and Multicomplexity) of caring for older surgical patients.
- Perform an assessment for delirium, initiate work-up for precipitating factors, treat underlying causes, and develop a safe care plan.
- Recognize risk factors for falls and fractures and create a plan for optimizing mobility.
- Perform a full medication reconciliation and identify medications that are potentially inappropriate.
- Summarize how to coordinate a safe and effective care transition for older patients, caregivers, and families
- Assess what matters most to older patients and apply these priorities into surgical planning.
- Associate geriatric syndromes such as frailty and dementia with adverse postoperative outcomes.
Thursday, March 14, 2024 | 11:00 AM - 4:00 PM ET
| 11:00am | Introduction to Day 1 - Surgery in Older Adults: An Age-Friendly Approach | Zara Cooper, MD, MSc |
11:15 | Mentation: Preventing & Addressing Delirium in Surgical Patients | Sevdenur Cizginer, MD, MPH, AGSF |
12:00pm | Medications: Polypharmacy & Deprescribing for Surgical Patients | Laura Frain, MD, MPH |
12:45 | Parallel Case-Based Workshops A) Delirium & Dementia Surgical Cases | Sharon Levine, MD & Deborah Lee, MD B) Medications: Geriatric Surgical Cases | Andrea Wershof Schwartz, MD, MPH & Lynne O'Mara, MPAS, PA-C |
| 1:15 | Break |
| 1:45 | Rehab, Prehab & Falls: Optimizing Mobility throughout the Surgical Continuum | Julia Loewenthal, MD & Nancy Latham, PhD |
| 2:30 | What Matters Most: Addressing Goals & Priorities for Surgical Patients | Elizabeth Lilley, MD, MPH |
| 3:15 | Parallel Case-Based Workshops A) Serious Illness Conversations: A Guide for Communication about Goals of Care | Rachelle Bernacki, MD, MS & Elizabeth Lilley, MD, MPH B) Supporting Caregivers & Surrogates Before, During & After Surgery | Tamryn Gray, PhD, RN, MPH & Zara Cooper, MD, MSc |
| 3:45 | Take Home Lessons for Geriatric Care | Andrea Schwartz, MD, MPH |
| 4:00pm | Adjournment |
Friday, March 15, 2024 | 11:00 AM - 4:30 PM ET
| 11:00am | Introduction to Day 2: Navigating Multicomplexity in Older Surgical Patients | Rachelle Bernacki, MD, MS |
| 11:15 | Peri-Operative Evaluation for Geriatric Surgery Patients | Rachelle Bernacki, MD, MS & Christine Cauley, MD, MPH |
| 12:00pm | Anesthesia & Pain Management in Older Surgical Patients | Stacie Deiner, MD |
| 12:45 | Parallel Case-Based Workshops A) Pre-Operative Evaluation & Pre-Habilitation | Christine Cauley, MD, MPH & Esteban Franco Garcia, MD B) Surgical Pain Management for Older Adults | Stacie Deiner, MD |
| 1:15 | Break |
| 1:45 | Frailty in Older Surgical Patients | Ariela Orkaby, MD, MPH |
| 2:30 | Multicomplexity: Considering Transitions of Care & Payment Models for Geriatric Surgery Patients | Esteban Franco Garcia, MD |
| 3:15 | Panel Discussion: Implementing Geriatric Surgery Care Models | Amy Bulger, RN, MPH, GERO-BC, CPHQ, Lynne O'Mara, MPAS, PA-C, Houman Javedan, MD, Roman Belenkiy, PharmD, BCGP & Masaya Higuchi, MD, MPH, CMD, AGSF |
| 4:15 | Course Wrap-Up | Andrea Schwartz, MD, MPH & Julia Loewenthal, MD |
| 4:30pm | Adjournment |
[format] => full_html ) [field_registration_instructions] => Array ( [value] =>
| Registration Type | Tuition Fee |
|---|---|
| Physicians | $375 |
| RNs, NPs & PAs | $275 |
| Trainees | Free |
Cancellation Policy:
Registrations cancelled on or before February 29, 2024 will be refunded, less a $45 administrative fee. Registrations cancelled after February 29, 2024 will not be refunded.
Contact partnerscpd@partners.org if you require assistance in cancelling your online registration.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for surgical clinicians, nurses, and physician assistants internal & external to the Mass General Brigham system.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3038 [id] => 3038 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Brigham & Women's Hospital - Department of Surgery & Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=52204
[first] => https://cpd.partners.org/node?nid=52204&page=0
[last] => https://cpd.partners.org/node?nid=52204&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this live activity for a maximum of 1.50 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 1.5 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
Physician Assistants
 Mass General Brigham has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 1.50 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation.
Mass General Brigham has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 1.50 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/231
[id] => 231
[resource] => taxonomy_term
[uuid] => 541dec03-c6af-4bcb-9af7-8fa28fedfb53
)
[1] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/232
[id] => 232
[resource] => taxonomy_term
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1662552000
[value2] => 1685851140
[duration] => 23299140
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1677621600
[value2] => 1683153000
[duration] => 5531400
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/239
[id] => 239
[resource] => taxonomy_term
[uuid] => 8fe8f562-9596-41a9-8e2f-c93aa2c8dae9
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/41510
[id] => 41510
[resource] => file
[uuid] => cdc59ac5-bffd-4758-9a58-2d1662885020
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => Please note, access to symposium recordings is included with registration.
Access will be available for 30 days post event.
With several new drug and cellular therapies as well as an expansion of our understanding of the biologic heterogeneity of hematologic malignancies, there is a need for ongoing education in the area of hematologic malignancies. This interactive webinar series will focus on current best practices and major updates in the biology, diagnosis, and management of hematologic malignancies.
Each 90-minute webinar will have two talks followed by 30 minutes of discussion and audience questions. Presenters will include internationally-known disease experts from Mass General Cancer Center covering practice-changing updates in cellular therapies, transplant, myeloma, leukemia, and lymphoma
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Course Director:
P. Connor Johnson, MD
Hematology/Oncology, Massachusetts General Hospital Cancer Center
Instructor in Medicine, Harvard Medical School
Faculty:
Jeremy Abramson, MD
Director, Jon and Jo Ann Hagler Center for Lymphoma, Massachusetts General Hospital Cancer Center
Associate Professor of Medicine, Harvard Medical School
Andrew Brunner, MD
Assistant Professor of Medicine, Harvard Medical School
Massachusetts General Hospital Cancer Center
Diana Cirstea, MD
Attending Physician
Multiple Myeloma Treatment Program
Massachusetts General Hospital Cancer Center
Zach DeFilipp, MD
Director, BMT Clinical Research, Massachusetts General Hospital Cancer Center
Assistant Professor of Medicine, Harvard Medical School
Areej El-Jawahri, MD
Associate Director, Cancer Outcomes Research and Education Program
Director, Bone Marrow Transplant Survivorship Program, Massachusetts General Hospital Cancer Center
Associate Professor of Medicine, Harvard Medical School
Matt Frigault, MD
Administrative Director, Cellular Therapy Service, Massachusetts General Hospital Cancer Center
Assistant Professor of Medicine, Harvard Medical School
Gaby Hobbs, MD
Clinical Director, Leukemia Service, Massachusetts General Hospital Cancer Center
Assistant in Medicine, Harvard Medical School
Noopur Raje, MD
Director, Center for Multiple Myeloma
Massachusetts General Hospital Cancer Center
Jake Soumerai, MD
Clinical Investigator in Lymphoma, Medicine, Massachusetts General Hospital
Assistant Professor, Medicine, Harvard Medical School
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Identify new therapies available for hematologic malignancies.
- Discuss practice-changing updates in the management of hematologic malignancies.
- Discuss new concepts in palliative care and survivorship.
- Determine appropriate timing to consider transplantevaluation and cellular therapy referral for hematologic malignancies.
[format] => full_html
)
[field_program] => Array
(
[value] => February 28, 2023 - Transplants
Speakers: Zach DeFilipp, MD & Areej El-Jawahri, MD
March 14, 2023 - Leukemia
Speakers: Andrew Brunner, MD & Gaby Hobbs, MD
March 22, 2023 - Cellular Therapies
Speakers: Jeremy Abramson, MD & Matt Frigault, MD
April 12, 2023 - Myeloma
Speakers: Diana Cirstea, MD & Noopur Raje, MD
May 3, 2023 - Lymphoma
Speakers: P. Connor Johnson, MD & Jake Soumerai, MD
[format] => full_html
)
[field_registration_instructions] => Array
(
[value] => CANCELLATION POLICY:
Registrations cancelled on or before February 14, 2023 will be refunded, less a $20 administrative fee. Registrations cancelled after Februrary 14, 2023 will not be refunded.
[summary] =>
[format] => full_html
)
[field_related_courses] => Array
(
)
[field_requirements_max] =>
[field_requirements_min] =>
[field_show_child_catalog] =>
[field_show_child_transcript] =>
[field_target_audience] => Array
(
[value] => This activity is intended for physicians, nurses, physician assistants, other members of healthcare team (regional) with specialties such as general practice, hematology, hematology/oncology, medical oncology, primary care, and radiation oncology.
[format] => full_html
)
[field_venue_phone] => Array
(
)
[upload] => Array
(
)
[field_accme_data] => Array
(
[uri] => https://cpd.partners.org/accme_data/2314
[id] => 2314
[resource] => accme_data
)
[field_show_on_calendar] =>
[field_custom_provided] => Array
(
[value] => Massachusetts General Hospital Cancer Center & Mass General Brigham
[summary] =>
[format] => full_html
)
[field_course_exhibitor] => Array
(
)
[field_course_qualifiers] => Array
(
)
[field_course_image_cards] => Array
(
)
[field_income_expense] => Array
(
)
[og_membership] => Array
(
)
[og_membership__1] => Array
(
)
[og_membership__2] => Array
(
)
[og_membership__3] => Array
(
)
[og_group_ref__og_membership] => Array
(
)
[og_group_ref__og_membership__1] => Array
(
)
[og_group_ref__og_membership__2] => Array
(
)
[og_group_ref__og_membership__3] => Array
(
)
[flag_course_bookmark_user] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/user/101228
[id] => 101228
[resource] => user
[uuid] => fe6daa11-5689-4a4e-8931-18476691e8f4
)
[1] => Array
(
[uri] => https://cpd.partners.org/user/30238
[id] => 30238
[resource] => user
[uuid] => 365971d5-0f3e-4b29-a012-bbae7e9ee8a7
)
[2] => Array
(
[uri] => https://cpd.partners.org/user/46019
[id] => 46019
[resource] => user
[uuid] => 419ba2f5-1f18-4be8-a630-7266d7ca92e9
)
)
[model] => course_52204
[list_price] => 0.00000
[cost] => 0.00000
[sell_price] => 149.00000
[price] => 149.00000
[weight] => 0
[weight_units] => lb
[length] => 0
[width] => 0
[height] => 0
[length_units] => in
[pkg_qty] => 1
[ordering] => 0
[shippable] => 0
[nid] => 52204
[vid] => 182199
[is_new] =>
[type] => course
[title] => Mass General Cancer Center Practice-Changing Updates in Hematologic Malignancies
[language] => und
[url] => https://cpd.partners.org/content/mass-general-cancer-center-practice-changing-updates-hematologic-malignancies
[edit_url] => https://cpd.partners.org/node/52204/edit
[status] => 1
[promote] => 1
[sticky] => 1
[created] => 1662554346
[changed] => 1705431039
[author] => Array
(
[uri] => https://cpd.partners.org/user/316
[id] => 316
[resource] => user
[uuid] => d6db325c-6680-48ed-a601-f114e3fb592a
)
[log] =>
[revision] =>
[course] => Array
(
[uri] => https://cpd.partners.org/course/52204
[id] => 52204
[resource] => course
)
[book_ancestors] => Array
(
)
[comment] => 1
[comments] => Array
(
)
[comment_count] => 0
[comment_count_new] => 0
[body] => Array
(
)
[feeds_item_guid] =>
[feeds_item_url] =>
[feed_nid] =>
[relation_faculty_user] => Array
(
)
[uuid] => fe80d13f-778f-4024-9c4a-58717b940d77
[vuuid] => 9cf14b65-56ad-4e06-8d96-7666753c638b
)
)
)
Array
(
[self] => https://cpd.partners.org/node?nid=62895
[first] => https://cpd.partners.org/node?nid=62895&page=0
[last] => https://cpd.partners.org/node?nid=62895&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this live activity for a maximum of 6.00 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 6.00 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
Physician Assistants
Mass General Brigham has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 6.00 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation

Lifelong Learning Maintenance of Certification (MOC) Program
MOC RECOGNITION STATEMENT
Successful completion of this CME activity, which includes participation in the evaluation component, enables the learner to earn credit toward the CME requirement of the American Board of Surgery’s Continuous Certification program. It is the CME activity provider's responsibility to submit learner completion information to ACCME for the purpose of granting ABS credit.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1690372800
[value2] => 1706738400
[duration] => 16365600
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1697801400
[value2] => 1697832000
[duration] => 30600
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/54991
[id] => 54991
[resource] => file
[uuid] => 73317cf9-4fdd-4765-962c-7990fe19ea61
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 44794
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Joseph B. Martin Conference Center
[street] => 77 Avenue Louis Pasteur
[additional] =>
[city] => Boston
[province] => MA
[postal_code] => 02115
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => This all-day event will promote the collaboration and interprofessional discussion regarding current innovative techniques and treatments. It will address the current debate surrounding approaches to the mitral valve: catheter-based procedures vs. open heart surgery. While there is some resistance to the use of catheter-based procedures in the treatment of mitral valve disease, this is mostly due to an existing stigma that assumes the old way is the best way. Historically, mitral valvuloplasty has been primarily treated with open heart surgery, but advancements in technology over the last century have allowed us to apply new techniques for disease treatment. The ongoing debate of which treatment is better (surgery or catheter based) is present in both fields. By the end of the event, attendees will be able to distinguish between the different approaches to the management of mitral valve disease and utilize procedures from both cardiac surgery and cardiology to better their practice in the future.
Please note that there are varying tuition prices:
| Registration Type | Tuition Fee |
|---|---|
| Physicians | $150 |
| Nurses & PAs | $100 |
| Fellows, Trainees & Learners | $50 |
(In Order of Appearance)
Mark J. Cunningham, M.D. - Course Director
Cardiac Surgery
Interim Chief, Cardiac Surgery
Brigham and Women’s Hospital
Robert S.D. Higgins, M.D., M.S.H.A.
Cardiac Surgery
President, Brigham and Women’s Hospital
Executive Vice President, Mass General Brigham
Thoralf Sundt, III., M.D.
Cardiac Surgery
Director, Cardiac Surgery Service Line
Mass General Brigham
Patrick T. O’Gara, M.D.
Cardiovascular Medicine
Watkins Family Distinguished Chair in Cardiology
Brigham & Women’s Hospital
Pinak Bipin Shah, M.D.
Cardiovascular Medicine
Director, Cardiac Catheterization Laboratory
Brigham and Women’s Hospital
Eugene Braunwald, M.D.
Cardiovascular Medicine
Distinguished Hersey Professor of Medicine, Harvard Medical School
Chairman Emeritus, Department of Medicine, Brigham and Women’s Hospital
Tirone David M.D., F.R.C.S.C.
Cardiac Surgery
Chief of Cardiac Surgery, University of Toronto
Melanie Munk Chair of Cardiovascular Surgery, Peter Munk Cardiac Centre
Stanton K. Shernan, M.D., F.A.H.A., F.A.S.E.
Cardiovascular Medicine
Benjamin G. Covino Professor of Anaesthesia
Brigham and Women’s Hospital
Tommaso Danesi, M.D.
Cardiac Surgery
Vice-Chief of Cardiac Surgery
AULSS 8, San Bortolo Hospital
Richard J. Shemin, M.D.
Cardiac Surgery
Robert & Kelly Day Chair in Cardiothoracic Surgery
University of California, Los Angeles
Gerard M. Doherty, M.D.
Surgeon-in-Chief
Crowley Family Distinguished Chair, Brigham and Women’s Hospital
[format] => full_html ) [field_hardware_software] => Array ( ) [field_hotel_information] => Array ( ) [field_hotel_link] => Array ( ) [field_hotel_photo] => Array ( ) [field_hotel_travel] => Array ( ) [field_learning_objectives] => Array ( [value] =>
Upon completion of this activity, participants will be able to:
- Reflect on the history of the mitral valvuloplasty.
- Contrast the different mitral valve procedures.
- Evaluate the future innovations of the procedure.
- Compare and contrast the different approaches to treating mitral valve disease, and how their practice could improve using different procedures.
| Time | Topic & Speaker |
|---|---|
| 8:00 AM | Introductions |
| 8:30 | History of Mitral Valve Interventions / Mitral Valve Management |
9:00 | Malignant Arrhythmia Syndrome |
| 9:30 | Transcatheter Mitral Valve Replacement / TEER |
| 10:00 | Break |
| 10:15 | Braunwald Video |
| 10:30 | Cutler Procedure |
| 11:00 | Mitral Valvuloplasty Procedure |
| 12:00 PM | Lunch Break |
1:00 | Multi-Modality Imaging Stanton Shernan, MD |
| 1:30 | Endoscopic Mitral Valve Repair |
2:00 | Break |
| 2:15 | History of Mitral Valve Repair at BWH: A Personal Journey |
| 3:15 | Concluding Remarks Gerard Doherty, MD |
| 3:30 PM | Adjournment |
| Registration Type | Tuition Fee |
|---|---|
| Physicians | $150 |
| Nurses & PAs | $100 |
| Fellows, Trainees & Learners | $50 |
Cancellation Policy:
Registrations cancelled on or before October 6, 2023 will be refunded, less a $15 administrative fee. Registrations cancelled after October 6, 2023 will not be refunded.
This activity is intended for Cardiac Surgery, Cardiology, and any other interested Physicians, Nurses, and Physician Assistants.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/2891 [id] => 2891 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Brigham & Women's Hospital, and Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=53573
[first] => https://cpd.partners.org/node?nid=53573&page=0
[last] => https://cpd.partners.org/node?nid=53573&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this live activity for a maximum of 7.00 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 7.00 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity
PAs
 Mass General Brigham has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 7.00 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation.
Mass General Brigham has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 7.00 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/231
[id] => 231
[resource] => taxonomy_term
[uuid] => 541dec03-c6af-4bcb-9af7-8fa28fedfb53
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1664211600
[value2] => 1680926340
[duration] => 16714740
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1676394000
[value2] => 1676493900
[duration] => 99900
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/239
[id] => 239
[resource] => taxonomy_term
[uuid] => 8fe8f562-9596-41a9-8e2f-c93aa2c8dae9
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/41509
[id] => 41509
[resource] => file
[uuid] => 26bc2951-6b98-4ebc-a9bc-6f30127a6cb4
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => Please note, access to symposium recordings is included with registration.
Access will be available for 30 days post event.
The Mass General Cancer Center Classical Hematology Review and ASH Highlights will be an interactive, virtual CME program highlighting state-of-the-art care for patients with hematologic diseases. This is a unique course, focused solely on classical hematology and the intricacies that come along with these diseases. Presentations will provide a combination of consultative case studies, approaches to patient care with various abnormalities, and the latest science and treatment paradigms from the 2022 ASH Meeting. There will be designated time in each section for a moderated Q&A, encouraging interaction between the audience and faculty.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Annemarie Fogerty, MD - Course Director
Assistant Professor of Medicine, Harvard Medical School
Massachusetts General Hospital Cancer Center
Hanny Al-Samkari, MD
Classical Hematologist and Clinical Investigator
Co-Director, Hereditary Hemorrhagic Telangiectasia Center
Massachusetts General Hospital
Assistant Professor of Medicine, Harvard Medical School
Sharl Azar, MD
Medical Director, Comprehensive Sickle Cell Disease Treatment Center
Massachusetts General Hospital Cancer Center
Pavan Bendapudi, MD
MGH Division of Hematology and Blood Transfusion Service
Assistant Professor of Medicine, Harvard Medical School
Larissa Bornikova, MD
Instructor in Medicine, Hematology-Oncology, Harvard Medical School
Massachusetts General Hospital Cancer Center
Jonathan Carlson, MD, PhD
Physician Investigator (Cl), Mass General Cancer Center, Mass General Research Institute
Instructor in Medicine, Harvard Medical School
Assistant In Medicine, Hematology-Oncology, Massachusetts General Hospital
Sunny Dzik, MD
Associate Pathologist, Massachusetts General Hospital
Associate Professor of Pathology, Harvard Medical School
Katayoon Goodarzi, MD
Physician Investigator, Mass General Research Institute
Instructor in Medicine, Harvard Medical School
Assistant In Medicine, Massachusetts General Hospital Cancer Center
Rebecca Karp, MD
Co-Founder and Co-Director, Porphyria Center
Assistant Professor, Harvard Medical School
Division of Hematology, Massachusetts General Hospital Cancer Center
David Kuter, MD, DPhil
Hematology Program Director, Massachusetts General Hospital
Professor of Medicine, Harvard Medical School
Rachel Rosovsky, MD, MPH
Director, Thrombosis Research - Division of Hematology, Massachusetts General Hospital Cancer Center
Co-Chair of Thrombosis Committee, Massachusetts General Hospital
Associate Professor, Harvard Medical School
David Sykes, MD, PhD
Assistant Professor, Harvard Medical School
Massachusetts General Hospital Cancer center
Anem Waheed, MD, MPH
Instructor in Medicine, Massachusetts General Hospital Cancer Center
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Identify and initiate management for a wide spectrum of hematology diseases
- Recognize emergent hematologic processes
- Operate appropriate diagnostic studies and initiate therapy
Cancellation Policy:
Registrations cancelled on or before January 31, 2023 will be refunded, less a $20 administrative fee. Registrations cancelled after January 31, 2023 will not be refunded.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>
This activity is intended for Physicians, Nurses, Physician Assistants and other members of the healthcare team across the United States.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/2372 [id] => 2372 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital Cancer Center & Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=54701
[first] => https://cpd.partners.org/node?nid=54701&page=0
[last] => https://cpd.partners.org/node?nid=54701&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => enrolled
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => This activity does not include CME credit.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1667998800
[value2] => 1704085140
[duration] => 36086340
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/237
[id] => 237
[resource] => taxonomy_term
[uuid] => 842d3b08-d27d-4a11-8281-71bcfb00ec51
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/41568
[id] => 41568
[resource] => file
[uuid] => 142c0644-765f-4aa1-9435-7ae66b267e7b
)
)
[field_course_intro] => Array
(
)
[field_course_live] =>
[field_course_location] => Array
(
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => The goal of this activity is to provide learners with a better understanding of immune mechanisms related to the pathogenesis of autoimmunity and rheumatoid arthritis. This module incorporates clinical scenarios and immunologic basic principles. In the module, learners acquire basic science knowledge, and then apply their understanding of JAK-kinase inhibition to the clinical management of patients. There is no fee for the online module.
We will provide collective feedback on module questions as value added to your participation.
The innovative adaptive learning platform used for this module will present content customized to each learner depending on baseline level of expertise. Depending on your baseline level of expertise, the module can be completed in as little as 30 minutes. The module may be completed in a single session or in small portions over time and may be accessed from any device.
Instructions to Complete the Module:
- Click on the blue "Register/Take Course" tab above
- You will be prompted to log in or register
- After you log in or register, we will receive notification of your enrollment
- We will email you a deidentified username, password and link to the adaptive learning module within 1 business day
- Use the login information provided by email to select and complete the module
- Provide any feedback
Target Audience
This activity is intended for physicians and advanced practice providers in the field of rheumatology. Dermatologists and gastroenterologists are a secondary target audience.
Additional Background Information:
This is an educational research project conducted by the Mass General Brigham Office of Professional Development Knowledge Translation Lab. Dr. Robert Birnbaum is the Principal Investigator, and Dr. Simon Helfgott is the Subject Matter Expert. All information derived from this study and data produced from your participation will be confidential. Data will be de-identified to protect healthcare provider information accessed by any constituencies. Data is collected for evaluating the efficacy of the learning methodology and to discern training needs — not to supervise or determine the level of your individual clinical acumen or skills. This educational research project is supported by funding from Eli Lilly. The content was solely developed by subject matter experts at Mass General Brigham.
Contact
Please contact us at partnerscpd@partners.org.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Course Director:
Robert J. Birnbaum, MD, PhD
Vice President, Continuing Professional Development, Mass General Brigham
Assistant Professor, Psychiatry, Harvard Medical School
Subject Matter Expert:
Simon Helfgott, MD
Director of Education & Fellowship Training, Brigham and Women's Hospital
Associate Professor of Medicine, Division of Rheumatology, Inflammation and Immunity, Harvard Medical School
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
)
[field_program] => Array
(
)
[field_registration_instructions] => Array
(
)
[field_related_courses] => Array
(
)
[field_requirements_max] =>
[field_requirements_min] =>
[field_show_child_catalog] =>
[field_show_child_transcript] =>
[field_target_audience] => Array
(
[value] => This activity is intended for rheumatologists, gastroenterologists, and dermatologists.
[format] => full_html
)
[field_venue_phone] => Array
(
)
[upload] => Array
(
)
[field_accme_data] => Array
(
[uri] => https://cpd.partners.org/accme_data/2442
[id] => 2442
[resource] => accme_data
)
[field_show_on_calendar] =>
[field_custom_provided] => Array
(
[value] => Mass General Brigham
[summary] =>
[format] => full_html
)
[field_course_exhibitor] => Array
(
)
[field_course_qualifiers] => Array
(
)
[field_course_image_cards] => Array
(
)
[field_income_expense] => Array
(
)
[og_membership] => Array
(
)
[og_membership__1] => Array
(
)
[og_membership__2] => Array
(
)
[og_membership__3] => Array
(
)
[og_group_ref__og_membership] => Array
(
)
[og_group_ref__og_membership__1] => Array
(
)
[og_group_ref__og_membership__2] => Array
(
)
[og_group_ref__og_membership__3] => Array
(
)
[flag_course_bookmark_user] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/user/36242
[id] => 36242
[resource] => user
[uuid] => 52b01039-6d57-4de5-acbf-6b8d847ec580
)
)
[model] => course_54701
[list_price] => 0.00000
[cost] => 0.00000
[sell_price] => 0.00000
[price] => 0.00000
[weight] => 0
[weight_units] => lb
[length] => 0
[width] => 0
[height] => 0
[length_units] => in
[pkg_qty] => 1
[ordering] => 0
[shippable] => 0
[nid] => 54701
[vid] => 147189
[is_new] =>
[type] => course
[title] => Rheumatoid Arthritis: The JAK/STAT Pathway and Clinical Autoimmunity
[language] => und
[url] => https://cpd.partners.org/content/rheumatoid-arthritis-jakstat-pathway-and-clinical-autoimmunity
[edit_url] => https://cpd.partners.org/node/54701/edit
[status] => 1
[promote] => 0
[sticky] => 0
[created] => 1667999626
[changed] => 1677875508
[author] => Array
(
[uri] => https://cpd.partners.org/user/1222
[id] => 1222
[resource] => user
[uuid] => f45a3401-52c1-4db6-a593-ccdf0f9de846
)
[log] =>
[revision] =>
[course] => Array
(
[uri] => https://cpd.partners.org/course/54701
[id] => 54701
[resource] => course
)
[book_ancestors] => Array
(
)
[comment] => 1
[comments] => Array
(
)
[comment_count] => 0
[comment_count_new] => 0
[body] => Array
(
)
[feeds_item_guid] =>
[feeds_item_url] =>
[feed_nid] =>
[relation_faculty_user] => Array
(
)
[uuid] => b36a884d-c1d0-4d81-bd42-6843320a6357
[vuuid] => 0f963507-e453-48cc-bec4-4d339f99974e
)
)
)
Array
(
[self] => https://cpd.partners.org/node?nid=68208
[first] => https://cpd.partners.org/node?nid=68208&page=0
[last] => https://cpd.partners.org/node?nid=68208&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this live activity for a maximum of 1.50 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 1.5 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
Pharmacy
This activity provides 1.5 contact hours (1.5 CEUs) of continuing education credit. ACPE Universal Activity Number (UAN): JA0007437-0000-24-001-L01-P
Pharmacy Technicians
This activity provides 1.5 contact hours (1.5 CEUs) of continuing education credit. ACPE Universal Activity Number (UAN): JA0007437-0000-24-001-L01-T
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/231
[id] => 231
[resource] => taxonomy_term
[uuid] => 541dec03-c6af-4bcb-9af7-8fa28fedfb53
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1701262800
[value2] => 1719806340
[duration] => 18543540
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1706824800
[value2] => 1716330600
[duration] => 9505800
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/7
[id] => 7
[resource] => taxonomy_term
[uuid] => 2a38b69f-4c76-44b0-bde5-67e901205c53
)
[1] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/239
[id] => 239
[resource] => taxonomy_term
[uuid] => 8fe8f562-9596-41a9-8e2f-c93aa2c8dae9
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/41510
[id] => 41510
[resource] => file
[uuid] => cdc59ac5-bffd-4758-9a58-2d1662885020
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => Please note, access to symposium recordings is included with registration.
Access will be available for 30 days post event.
With several new drug and cellular therapies as well as an expansion of our understanding of the biologic heterogeneity of hematologic malignancies, there is a need for ongoing education in the area of hematologic malignancies. This interactive webinar series will focus on current best practices, and how those are evolving based on major updates in the biology, diagnosis, and management of hematologic malignancies. Attendee interaction is encouraged and promoted through the designated time for audience questions at the end of each webinar. Each 90-minute webinar will have two talks followed by discussion and audience Q&A. Presenters will include internationally-known disease experts from Mass General Cancer Center covering high-yield practice-changing updates in cellular therapies, transplant, myeloma, leukemia, and lymphoma.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Course Director:
P. Connor Johnson, MD
Hematology/Oncology, Massachusetts General Hospital Cancer Center
Instructor in Medicine, Harvard Medical School
Faculty:
Andrew Brunner, MD
Assistant in Medicine, Center for Leukemia, Massachusetts General Hospital;
Assistant Professor, Medicine, Harvard Medical School
Diana Cirstea, MD
Attending Physician, Center for Multiple Myeloma
Massachusetts General Hospital Cancer Center
Zach DeFilipp, MD
Director, BMT Clinical Research, Massachusetts General Hospital Cancer Center
Assistant Professor of Medicine, Harvard Medical School
Matt Frigault, MD
Administrative Director, Cellular Therapy Service, Massachusetts General Hospital Cancer Center
Assistant Professor of Medicine, Harvard Medical School
Erika Haydu, MD, PhD
Assistant in Medicine, Massachusetts General Hospital
Instructor in Medicine, Harvard Medical School
Gaby Hobbs, MD
Clinical Director, Leukemia Service, Massachusetts General Hospital Cancer Center
Assistant in Medicine, Harvard Medical School
Richard Newcomb, MD
Instructor of Medicine, Harvard Medical School
Assistant Physician, Massachusetts General Hospital
Jake Soumerai, MD
Clinical Investigator in Lymphoma, Medicine, Massachusetts General Hospital
Assistant Professor, Medicine, Harvard Medical School
Andrew Yee, MD
Clinical Director, Center for Multiple Myeloma
Massachusetts General Hospital Cancer Center
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Describe new therapies available for hematologic malignancies.
- Discuss practice-changing updates in the management of hematologic malignancies Consider new concepts in palliative care and survivorship.
- Determine appropriate timing to consider transplant evaluation and cellular therapy referral for hematologic malignancies.
- Discuss latest and most promising disease-specific treatment options amongst the team to improve patient outcomes.
FUNDING
Mass General Cancer Center Practice-Changing Updates in Hematologic Malignancies 2024 has received support in the form of an educational grant from the following companies:
AbbVie Inc.
AstraZeneca Pharmaceuticals
Bristol Myers Squibb
Incyte Corporation
[format] => full_html
)
[field_program] => Array
(
[value] => February 1, 2024 - Lymphoma
Speakers: Jake Soumerai, MD & Erika Haydu, MD, PhD
February 26, 2024 - Cellular Therapies
Speakers: Matthew Frigault, MD & P. Connor Johnson, MD
March 27, 2024 - Myeloma
Speakers: Andrew Yee, MD & Diana Cirstea, MD
April 23, 2024 - Leukemia
Speakers: Gaby Hobbs, MD & Andrew Brunner, MD
May 21, 2024 - Transplants
Speakers: Zachariah DeFilipp, MD & Richard Newcomb, MD
[format] => full_html
)
[field_registration_instructions] => Array
(
[value] => CANCELLATION POLICY:
Registrations cancelled on or before February 12, 2024 will be refunded, less a $20 administrative fee. Registrations cancelled after February 12, 2024 will not be refunded.
[summary] =>
[format] => full_html
)
[field_related_courses] => Array
(
)
[field_requirements_max] =>
[field_requirements_min] =>
[field_show_child_catalog] =>
[field_show_child_transcript] =>
[field_target_audience] => Array
(
[value] => This activity is intended for physicians, nurses, pharmacists, other members of healthcare team (regional) with specialties such as general practice, hematology, hematology/oncology, medical oncology, primary care, and radiation oncology.
[format] => full_html
)
[field_venue_phone] => Array
(
)
[upload] => Array
(
)
[field_accme_data] => Array
(
[uri] => https://cpd.partners.org/accme_data/3052
[id] => 3052
[resource] => accme_data
)
[field_show_on_calendar] =>
[field_custom_provided] => Array
(
[value] => Massachusetts General Hospital Cancer Center & Mass General Brigham
[summary] =>
[format] => full_html
)
[field_course_exhibitor] => Array
(
)
[field_course_qualifiers] => Array
(
)
[field_course_image_cards] => Array
(
)
[field_income_expense] => Array
(
)
[og_membership] => Array
(
)
[og_membership__1] => Array
(
)
[og_membership__2] => Array
(
)
[og_membership__3] => Array
(
)
[og_group_ref__og_membership] => Array
(
)
[og_group_ref__og_membership__1] => Array
(
)
[og_group_ref__og_membership__2] => Array
(
)
[og_group_ref__og_membership__3] => Array
(
)
[flag_course_bookmark_user] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/user/58053
[id] => 58053
[resource] => user
[uuid] => 39bddd71-3630-481f-9608-7074dc17351e
)
[1] => Array
(
[uri] => https://cpd.partners.org/user/130233
[id] => 130233
[resource] => user
[uuid] => 740ada15-c08c-4a1f-ac15-2bac28c17e6d
)
[2] => Array
(
[uri] => https://cpd.partners.org/user/77843
[id] => 77843
[resource] => user
[uuid] => 81974fc8-b3df-41cc-a65f-efc5f26638c2
)
[3] => Array
(
[uri] => https://cpd.partners.org/user/13623
[id] => 13623
[resource] => user
[uuid] => 99174dc0-ee8c-4afb-9a25-a8f8e52f9193
)
[4] => Array
(
[uri] => https://cpd.partners.org/user/77793
[id] => 77793
[resource] => user
[uuid] => 5759ed92-18d9-4e66-b025-c625ac31b467
)
)
[model] => course_68208
[list_price] => 0.00000
[cost] => 0.00000
[sell_price] => 149.00000
[price] => 149.00000
[weight] => 0
[weight_units] => lb
[length] => 0
[width] => 0
[height] => 0
[length_units] => in
[pkg_qty] => 1
[ordering] => 0
[shippable] => 0
[nid] => 68208
[vid] => 185722
[is_new] =>
[type] => course
[title] => Mass General Cancer Center Practice-Changing Updates in Hematologic Malignancies 2024
[language] => und
[url] => https://cpd.partners.org/content/mass-general-cancer-center-practice-changing-updates-hematologic-malignancies-2024
[edit_url] => https://cpd.partners.org/node/68208/edit
[status] => 1
[promote] => 1
[sticky] => 1
[created] => 1699451212
[changed] => 1708968863
[author] => Array
(
[uri] => https://cpd.partners.org/user/92
[id] => 92
[resource] => user
[uuid] => 48adffb8-b573-4cd5-ada8-52d9bb7f0770
)
[log] =>
[revision] =>
[course] => Array
(
[uri] => https://cpd.partners.org/course/68208
[id] => 68208
[resource] => course
)
[book_ancestors] => Array
(
)
[comment] => 1
[comments] => Array
(
)
[comment_count] => 0
[comment_count_new] => 0
[body] => Array
(
)
[feeds_item_guid] =>
[feeds_item_url] =>
[feed_nid] =>
[relation_faculty_user] => Array
(
)
[uuid] => ee274591-fbe4-425d-a15a-694ec19e36eb
[vuuid] => 02aa0d53-cc24-47d1-9149-3353ee50f588
)
)
)
Array
(
[self] => https://cpd.partners.org/node?nid=75641
[first] => https://cpd.partners.org/node?nid=75641&page=0
[last] => https://cpd.partners.org/node?nid=75641&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this live activity for a maximum of 14.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 14.5 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
Physician Assistants
Mass General Brigham has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 14.5 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation.

[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1721043600
[value2] => 1734065940
[duration] => 13022340
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1731326400
[value2] => 1731445200
[duration] => 118800
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/238
[id] => 238
[resource] => taxonomy_term
[uuid] => fd81c17a-d19b-46b8-ad6b-2c5aee9ce9be
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/71052
[id] => 71052
[resource] => file
[uuid] => 30bc389b-bdb0-4d9d-897b-c2f8a4841a23
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 53790
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Fairmont Copley Hotel
[street] => 138 St James Ave
[additional] =>
[city] => Boston
[province] => MA
[postal_code] => 02116
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => The care of injured and critically ill patients is complex and challenging. The goal for the Trauma and Acute Care Surgery Symposium at Massachusetts General Hospital, aims to give clear guidelines to practicing clinicians who manage such patients. This symposium offers an ideal mix of the traditional standard-of-care principles with new, cutting-edge information. It explores issues in several areas including resuscitation, surgical techniques, bleeding control, inflammation and infection, respiratory care, nutrition, prehospital care, rehabilitation, and ethics. Multiple learning modalities will be incorporated into the course to engage the learner in the educational process and help them develop new strategies they can apply in their own practice setting.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Course Director
George Velmahos, MD
Division Chief of Trauma, Emergency Surgery and Surgical Critical Care,
Massachusetts General Hospital;
John F. Burke Professor of Surgery, Harvard Medical School
Faculty
Aalok Agarwala, MD
Division Chief, General Surgery Anesthesia,
Associate Director, Anesthesia Quality and Safety,
Massachusetts General Hospital
Katherine Albutt, MD
Department of Surgery,
Massachusetts General Hospital
Suzanne Algeri, RN
Associate Chief Nurse, Surgical, Orthopedics and Neurosciences,
Massachusetts General Hospital
Reza Askari, MD
Assistant Professor, Harvard Medical School;
Trauma, Burn and Surgical Critical Care,
Brigham and Women's Hospital
Matthew Bartek, MD
General Surgeon, Critical Care Physician,
Palliative Care Physician,
Massachusetts General Hospital
Salem Hospital
Kristina Bermas, MD
Medical Director, Acute Care Surgery and Trauma, Wentworth-Douglass Hospital
Surgical Director, Critical Care Unit, Wentworth-Douglass Hospital
Trauma, Emergency Surgery, and Surgical Critical Care, Massachusetts General Hospital
Gabriel Brat, MD
Assistant Professor of Surgery, Beth Israel Deaconess Medical Center;
Assistant Professor of Biomedical Informatics, Harvard Medical School (Secondary)
Gary Brenner, MD, PhD
Director, MGH Pain Medicine Fellowship,
Massachusetts General Hospital
Christopher Burns, MD
Division of Trauma, Burn and Surgical Critical Care,
Brigham and Women's Hospital
Jason Cohen, MD
Chief Medical Officer,
Boston MedFlight
Charles Cook, MD
Associate Professor of Surgery, Harvard Medical School;
Chief of Acute Care Surgery, Trauma, and Surgical Critical Care,
Beth Israel Deaconess Medical Center
Amory de Roulet, MD
General Surgeon,
Massachusetts General Hospital
Matthew Elson, MD
General Surgery,
Massachusetts General Hospital
Adam Field, MD
Clinical Fellow in Surgery,
Brigham and Women's Hospital
Karim Fikry, MD
Anesthesiology,
Surgical Critical Care,
Lahey Hospital & Medical Center
Jonathan Gates, MD
Chief, Surgery, Hartford Hospital
Denise Gee, MD
Vice Chair, Clinical Operations, Department of Surgery,
Surgical Director, Mass General Weight Center
Section Head, Swallowing, Heartburn and Esophageal Disease Program,
Massachusetts General Hospital
Petrut Gogalniceanu, MD
Guy's and St Thomas NHS Trust, King's College, United Kingdom
Robert Goldstone, MD
Colorectal Surgeon, Newton-Wellesley Hospital;
Staff Surgeon, Massachusetts General Hospital
Jeremy Goverman, MD
Burns Service,
Surgery,
Massachusetts General Hospital
Peter Hedberg, MD
General Surgeon,
Massachusetts General Hospital
Martha's Vineyard Hospital
Nir Hus, MD
Trauma Surgeon, Delray Beach Medical Center;
Assistant Professor of Surgery, Schmidt College of Medicine, Florida Atlantic University
Shams Iqbal, MBBS
Interventional Radiologist,
Massachusetts General Hospital
Megan Janeway, MD
Surgeon, Acute Care and Trauma Surgery/Surgical Critical Care,
Boston Medical Center (BMC);
Assistant Professor of Surgery, Boston University Chobanian & Avedisian School of Medicine (CASM)
Haytham Kaafarani, MD
Professor of Surgery, Harvard Medical School;
Medical Director, Hospital Quality & Safety,
Medical Director, Trauma Center,
Massachusetts General Hospital
Jane Keating, MD
Acute Care Surgery,
Hartford Hospital
Edward Kelly, MD
Chief, Division of Trauma, Acute Care Surgery & Surgery Critical Care,
Baystate Health
David King, MD
Trauma and Acute Care Surgeon,
Massachusetts General Hospital
David Lawlor, MD
Pediatric Surgery,
Mass General for Children
Michael Llwellyn, PA-C
Lead Physician Assistant for Robotic Surgery,
Department of Surgery,
Massachusetts General Hospital
Casey Luckhurst, MD
Pancreatic and General Surgeon
Inpatient Director, Pancreatitis Treatment Center,
Massachusetts General Hospital
Adrian Maung, MD
Associate Professor of Surgery (General, Trauma & Surgical Critical Care),
Trauma Medical Director, Surgery,
Surgical Director, Perioperative Services, Surgery
Yale School of Medicine
Fred Millham, MD
Chief of Surgery, South Shore Hospital
Lauren Nentwich, MD
Emergency Medicine Physician,
Boston Medical Center (BMC)
Josh Ng-Kamstra, MD
Surgeon,
Trauma, Emergency Surgery, and Surgical Critical Care,
Massachusetts General Hospital
Jonathan Parks, MD
General Surgery, Surgical Critical Care,
Massachusetts General Hospital
Martha's Vineyard Hospital
Erika Rangel, MD
Acute Care and General Surgeon
Associate Program Director, Surgical Residency Program,
Massachusetts General Hospital
Ali Salim, MD
Division Chief, Trauma, Burn and Surgical Critical Care,
BWH Distinguished Chair in Surgery,
Brigham and Women's Hospital
Professor of Surgery, Harvard Medical School
Sabrina Sanchez , MD
Associate Professor of Surgery
Associate Chair for Faculty Development and Diversity,
Boston University, Chobanian & Avedisian School of Medicie
Kevin Schuster, MD
Professor of Surgery (General, Trauma & Surgical Critical Care),
Section Chief, General Surgery, Trauma & Surgical Critical Care,
Yale School of Medicine
Jamie Sparling, MD
Director, Trauma & Burn Anesthesia,
Massachusetts General Hospital
Sarah Stokes, MD
Department of Surgery,
Beth Israel Deaconess Medical Center
Crisanto Torres, MD
Trauma Surgeon,
Boston Medical Center (BMC);
Assistant Professor of Surgery, Boston University Chobanian & Avedisian School of Medicine (CASM)
Robert Winchell, MD
G. Thomas Shires II Professor of Surgery,
Professor of Medical Ethics in Medicine,
Chief, Division of Trauma, Burns, Acute and Critical Care,
Weill Cornell Medicine
Sara Zhao, MD
Interventional Radiologist,
Associate Program Director, Interventional Radiology Residency Program,
Massachusetts General Hospital
Instructor, Harvard Medical School
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of the activity, participants will be able to:
- Apply treatment plans for trauma and acute surgery patients.
- Describe indications for operative versus non-operative management after complex emergency surgical problems.
- Evaluate challenges related to systems of, and leadership in, patient care.
- Create systems to improve quality of trauma care in their own institutions.
- Organize multidisciplinary teams to provide well-coordinated care.
Maintenance of Certification (MOC)
American Board of Surgery (ABS) MOC Recognition Statement
Successful completion of this CME activity, which includes participation in the evaluation component, enables the learner to earn credit toward the CME requirement of the American Board of Surgery’s Continuous Certification program. It is the CME activity provider's responsibility to submit learner completion information to ACCME for the purpose of granting ABS credit.
[format] => full_html
)
[field_program] => Array
(
[value] => Monday, November 11, 2024 | 7:00am - 4:40pm
Trauma & Critical Care
7:00am | Welcome | George Velmahos, MD |
Session I: DEBATES IN PREHOSPITAL TRAUMA CARE | |
7:15 | Mechanical v. Hand Chest Compression | Jason Cohen, MD |
7:30 | Blood Product Transfusion v. Traditional Fluids | Crisanto Torres, MD |
7:45 | Intubation v. Bag Valve Mask | Lauren Nentwich, MD |
8:00 | Discussion |
Session II: WE DISAGREE! - CLEARANCE OF THE C-SPINE | |
8:10 | MRI Is Needed To Clear It With Confidence | Adrian Maung, MD |
8:20 | CT is Good Enough If You Know How To Read It | Katherine Albutt, MD |
8:30 | Rebuttal/Discussion/Vote |
Session III: WE DISAGREE! - EVACUATION OF RETAINED HEMOTHORAX | |
8:40 | VATS is Efficient, Fast, The Best | Reza Askari, MD |
8:50 | Fibrinolytics Are Gentle, Safe, The Best | Sara Zhao, MD |
9:00 | Rebuttal/Discussion/Vote |
Session IV: WE DISAGREE! - REBOA FOR TEMPORARY BLEEDING CONTROL | |
9:10 | REBOA Saves Lives! | Jane Keating, MD |
9:20 | REBOA is a Passing Fad! | Christopher Burns, MD |
9:30 | Rebuttal/Discussion/Vote |
9:40 | BREAK |
Session V: TRAUMA JEOPARDY | |
10:00 | A Game of Trauma Knowledge and Fast Reflexes! | Matthew Elson, MD; Adam Fields, MD; Sarah Stokes, MD |
Session VI: THE IMPOSSIBLE TRAUMA OPERATION | |
10:40 | Pancreatic Resection v. Packing and Drainage | Casey Luckhurst, MD |
10:50 | Hepatic Repair v. Packing and Embolization | Edward Kelly, MD |
11:00 | Explore Always the Zone - Penetrating Retroperitoneal Injury? | Kevin Schuster, MD |
11:10 | Discussion |
Session VII: CHALLENGING TRAUMA POPULATIONS | |
11:20 | The Top 5 Differences of Pediatric Trauma Patients | David Lawlor, MD |
11:40 | The Top 5 Differences of Geriatric Trauma Patients | Sabrina Sanchez , MD |
11:50 | The Top 5 Differences of Pregnant Trauma Patients | Kristina Bermas, MD |
12:00pm | The Top 5 Differences of Superobese Trauma Patients | Peter Hedberg, MD |
12:20 | LUNCH |
Session VIII: A PANEL ON TRAUMA LEADERSHIP | |
1:30 | Can a Terrible Leader Be A Great Clinician? | Petrut Gogalniceanu, MD |
1:45 | Creating Order Out of Chaos in the Trauma Bay | Haytham Kaafarani, MD |
2:00 | What Type of a Leader Do We Want? | Discussion and Audience Participation |
Session IX: A PANEL ON QUALITY AND SAFETY | |
2:15 | Introduction | Haytham Kaafarani, MD |
2:20 | In-Hospital Never-Events: Truly Never? | Suzanne Algeri, RN & Laura Ream, RN |
2:30 | Zero Preventable Deaths: Truly Zero? | Robert Winchell, MD |
| 2:40 | Rescue Before The Rescue | Aalok Agarwala, MD |
2:50 | Discussion |
Session X: MODERN TRENDS IN.. | |
3:00 | Soft Tissue Reconstruction | Nir Hus, MD |
3:15 | Hemostatic Agents | David King, MD |
3:30 | Discussion |
Session XI: THE SURVIVOR GAME | |
3:40 | A Game of Mystery, Trauma Expertise, and Audience-Seducing Skills | Kevin Schuster, MD; Kristina Bermas, MD; Jane Keating, MD; Megan Janeway, MD; Nir Hus, MD |
4:40pm | Adjourn |
Tuesday, November 12, 2024 | 7:30am - 4:00pm
Acute Care Surgery
Session XII: WHAT'S NEW IN…. | |
7:30am | Perforated Diverticulitis | Robert Goldstone, MD |
7:40 | Necrotizing Pancreatitis | Casey Luckhurst, MD |
7:50 | Non-Operative Cholecystitis | Shams Iqbal, MBBS |
8:00 | Discussion |
Session XII: MESH OR NO MESH OR WHAT MESH? | |
8:15 | Small Umbilical Hernia: Elective or Strangulated | Reza Askari, MD |
8:30 | Contaminated/Infected Ventral Hernia | Jonathan Parks, MD |
8:45 | Parastomal Hernia: Elective or Strangulated | Josh Ng-Kamstra, MD |
9:00 | Discussion |
Session XIII: THE ONE QUESTION THAT MATTERS | |
9:15 | Enteral or Parenteral Nutrition? | Edward Kelly, MD |
9:25 | Which Wound Dressing? | Jeremy Goverman, MD |
9:35 | How to Come Off Anesthesia Without Coughing? | Jamie Sparling, MD |
9:45 | When to Give Anticoagulation Reversal? | Karim Fikry, MD |
9:55 | Discussion |
10:00 | BREAK |
Session XIV: THE MAGIC INTERVENTION IS… | |
10:30 | …Robotic Acute Care Surgery | Michael Llwellyn, PA-C |
10:40 | …Prediction/Prescription Through AI | Gabriel Brat, MD |
10:50 | …Surgical Palliative Care | Matthew Bartek, MD |
11:00 | …Home Hospital | Denise Gee, MD |
11:10 | Discussion |
Session XV: KEYNOTE LECTURE | |
11:25 | Introduction of the Keynote Lecturer | George Velmahos, MD |
11:30 | Memento Mori | Robert Winchell, MD |
12:00pm | LUNCH |
Session XVI: THE MAGIC DRUG IS… | |
1:00 | …Controls Persistent Pain | Gary Brenner, MD, PhD |
1:15 | …Controls Persistent Bleeding | Jonathan Gates, MD |
1:45 | …Controls Persistent Crisis | Petrut Gogalniceanu, MD |
2:00 | Discussion |
Session XVII: My Greatest Catastrophe (and the moral of the story) | |
2:15 | Case #1 - The Uncontrollable Leak | Edward Kelly, MD |
2:25 | Case #2 - The Impossible Bowel Fistula | Jonathan Parks, MD |
2:35 | Case #3 - The Supermobile Bowel | Amory de Roulet, MD |
2:45 | Discussion |
Session XVIII: LAST PERSON STANDING | |
3:00 | Trauma Knowledge From This Symposium - An Interactive Game with The Audience |
4:00pm | Adjourn |
[format] => full_html ) [field_registration_instructions] => Array ( [value] =>
| Tuition Type | Early Bird Tuition Fees (until September 18, 2024) | Regular Tuition Fees (after September 18, 2024) |
|---|---|---|
| Physician (MD/DO) | $800.00 | $850.00 |
| Nurse (RN/APRN) | $650.00 | $700.00 |
| Resident/Fellow | $550.00 | $600.00 |
| Allied Health Professional / Other | $650.00 | $700.00 |
Cancellation Policy:
Registrations cancelled on or before October 28, 2024 will be refunded, less a $90 administrative fee. Registrations cancelled after October 28, 2024 will not be refunded.
Contact partnerscpd@partners.org if you require assistance in cancelling your online registration.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for Physicians, Nurses, Nurse Practitioners, Physician Assistants, and other members of the healthcare team who focus on critical care, emergency medicine, general surgery and trauma/acute surgery.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3331 [id] => 3331 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital, and Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=55408
[first] => https://cpd.partners.org/node?nid=55408&page=0
[last] => https://cpd.partners.org/node?nid=55408&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 Credits™
Mass General Brigham designates this live activity for a maximum of 11.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 11.5 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
MOC COMPLETION CRITERIA
Participant completion for MOC points will be reported to the boards at the conclusion of the course.
Please have your ABIM ID available when completing the evaluation at the end of the course.
Instructions: Medical Knowledge MOC points in the American Board of Internal Medicine's (ABIM) Maintenance of Certification (MOC) Program
Upon successful completion of this activity, if you wish to receive MOC Part 2 points you will need to enter your ABIM ID number in the post-course evaluation. The Mass General Brigham Office of Continuing Professional Development will verify completion of your activity and report to the ABIM. Diplomates must check their ABIM Portfolio for confirmation of your MOC Part 2 points.
MOC Recognition Statement
Successful completion of this CME activity, which includes participation in the activity, with individual assessments of the participant and feedback to the participant, enables the participant to earn 11.5 MOC points in the American Board of Internal Medicine (ABIM) Maintenance of Certification (MOC) program. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/197
[id] => 197
[resource] => taxonomy_term
[uuid] => 621a8034-627c-4c33-b273-260b2d83768c
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1672842180
[value2] => 1690775940
[duration] => 17933760
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1682683200
[value2] => 1682784900
[duration] => 101700
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/239
[id] => 239
[resource] => taxonomy_term
[uuid] => 8fe8f562-9596-41a9-8e2f-c93aa2c8dae9
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/42381
[id] => 42381
[resource] => file
[uuid] => 32a35228-99d7-4e04-9fc2-f5daed3696ca
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 37092
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Livestream
[street] => Massachusetts General Hospital
[additional] =>
[city] => Boston
[province] => MA
[postal_code] => 02114
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => THIS IS A VIRTUAL COURSE

5C: Concepts in Contemporary Critical Care Cardiology is a novel offering of the MGH Heart Center designed to educate practicing clinicians about current topics at the forefront of cardiac intensive care – such as ECMO and mechanical circulatory support - and provide clinicians with a robust evidence base of medical knowledge to be able to provide comprehensive care to modern cardiac intensive care patients.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Course Directors
David Dudzinski, MD, JD

Assistant Professor of Medicine, Harvard Medical School;
Director of Cardiac Intensive Care Unit, Massachusetts General Hospital
Ivana Nikolic, MD

Instructor in Medicine, Harvard Medical School;
Cardiologist, Massachusetts General Hospital
Faculty
Aaron Aguirre, MD, PhD
Assistant Professor of Medicine, Harvard Medical School;
Critical Care Cardiologist, Massachusetts General Hospital
Aranya Bagchi, MBBS
Assistant Professor of Anesthesia, Harvard Medical School;
Anesthesiologist, Critical Care and Pain Medicine, Massachusetts General Hospital
Amit Bardia, MBBS
Anesthesiologist, Massachusetts General Hospital
Lisa Bebell, MD, MSc
Instructor of Medicine, Harvard Medical School;
Critical Care Medicine and Infectious Diseases, Massachusetts General Hospital
Marvin Chang, MD, PhD
Assistant Professor of Anesthesia, Harvard Medical School;
Anesthesiologist, Massachusetts General Hospital
Ryan Chung, MD
Massachusetts General Hospital
David Convissar, MD
Instructor in Anesthesia, Harvard Medical School;
Anesthesiologist, Critical Care and Pain Medicine, Massachusetts General Hospital
Jerome Crowley, MD, MPH
Instructor in Anesthesia, Harvard Medical School;
Cardiothoracic Anesthesiologist, Critical Care Medicine, Massachusetts General Hospital
Kyle Devins, MD
Massachusetts General Hospital
Danielle Doucette, RRT
Massachusetts General Hospital
Mike Fitzsimons, MD
Associate Professor of Anesthesia, Harvard Medical School;
Anesthesiologist, Critical Care and Pain Medicine, Massachusetts General Hospital
Kathryn Hibbert, MD
Assistant Professor of Medicine, Harvard Medical School;
Critical Care Cardiologist, Massachusetts General Hospital
Sohah Iqbal, MD
Chief of Interventional Cardiology,
Massachusetts General Hospital - Salem
Eric Isselbacher, MD
Associate Professor of Medicine, Harvard Medical School;
Co-Director, Thoracic Aortic Center, Massachusetts General Hospital
Yvonne Lai, MD
Assistant Professor of Anesthesia, Harvard Medical School;
Anesthesiologist, Critical Care Medicine, Massachusetts General Hospital
Dennis Lu, MD
Ina Ly, MD
Massachusetts General Hospital
Jona Ludmir, MD
Assistant Professor of Medicine, Harvard Medical School;
Critical Care Cardiologist, Massachusetts General Hospital
Rajeev Malhotra, MD, MS
Assistant Professor of Medicine, Harvard Medicine School;
Cardiologist, Massachusetts General Hospital
Ioannis Mastoris, MD
Advanced Heart Failure and Transplant Cardiologist, Mass General Brigham;
Instructor of Medicine, Harvard Medical School
Eriberto Michel, MD
Assistant Professor of Surgery, Harvard Medical School;
Cardio-Thoracic Surgeon, Massachusetts General Hospital
Jahan Mohebali, MD, MPH
Assistant Professor of Surgery, Harvard Medical School;
Cardio-Thoracic Surgeon, Massachusetts General Hospital
Christopher Newton-Cheh, MD, MPH
Massachusetts General Hospital
Philip Podrid, MD
Cardiac Electrophysiology, Boston Medical Center
Malavika Prabhu, MD
Massachusetts General Hospital
Jill Rackliffe, CNP
Massachusetts General Hospital
Jonah Rubin, MD
Massachusetts General Hospital
Marc Sabatine, MD, MPH
Professor of Medicine, Harvard Medical School;
Cardiologist, Massachusetts General Hospital
Kenneth Shelton, MD
Assistant Professor of Anesthesia, Harvard Medical School;
Chief, Division of Critical Care, Massachusetts General Hospital
Michael Silverman, MD, MPH
Assistant Professor of Medicine, Harvard Medical School;
Cardiac Critical Care Cardiologist, Massachusetts General Hospital
Edmond Solomon, RPh
Massachusetts General Hospital
Kelly Tankard, MD
Instructor of Medicine, Harvard Medical School;
Critical Care Anesthesiologist, Massachusetts General Hospital
Lana Tsao, MD
Instructor of Medicine, Harvard Medical School;
Heart Failure Cardiologist, Massachusetts General Hospital
Van-Khue Ton, MD, PhD
Assistant Professor of Medicine, Harvard Medical School;
Advanced Heart Failure & Transplantation Cardiologist, Massachusetts General Hospital
Mary Norine Walsh, MD
St. Vincent Heart Center
Alison Witkin, MD
Assistant Professor of Medicine, Harvard Medical School;
Associate Director of Pulmonary Hypertension and Thromboendarterectomy, Massachusetts General Hospital
Man Piu (Mark) Wong, MD
Instructor of Anesthesia, Harvard Medical School;
Anesthesiologist, Massachusetts General Hospital
Evin Yucel, MD
Instructor of Medicine, Harvard Medical School;
Cardiologist Specializing in Echocardiography, Massachusetts General Hospital
Emily Zern, MD
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Compare available strategies for urgent univentricular and biventricular mechanical support.
- Choose vasoactive medications based on an algorithmic approach to shock phenotypes.
- Practice consensus-based selection criteria for choosing ECMO and mechanical circulatory support strategies.
- Select strategies for optimal care of the post-arrest patient.
- Manage refractory hypoxemia with improved understanding of ventilator parameters and mechanics in cardiac patients, and acknowledge heart-lung interaction and impact on physiology and treatment.
- Evaluate contributions of right ventricular dysfunction and ventricular interdependence in acute cardiopulmonary dysfunction.
- Demonstrate appropriate systems-based practice in modern cardiac critical care by employing care bundles and evidence-based practice with nutrition and physical therapy.
- Recognize signs and causes of delirium in critically ill patients and implement appropriate neuropharmacologic treatment plan.
Social Media
Twitter:
Mass General Brigham Professional Development
@MassGenBrighCPD
MGH Corrigan Minehan Heart Center
@MGHHeartHealth
LinkedIn:
Mass General Brigham Professional Development
[format] => full_html
)
[field_program] => Array
(
[value] => Friday, April 28, 2023 | 7:50am - 4:30pm
| 7:50am | Welcome & Introduction | David M. Dudzinski, JD, MD; Ivana Nikolic, MD; Jill Rackliffe, NP |
Section I: Tools of the Trade | |
8:00 | Contemporary Cardiac Critical Care; Trends, Importance of Non-Cardiac Comorbidities in Modern Cardiac Critical Care | David M. Dudzinski, JD, MD |
8:15 | Shock Phenotypes, Vasoactive Agents for Complex Cardiovascular Scenarios | |
8:35 | EKG pearls for the cardiac ICU | Phil Podrid, MD |
8:55 | Getting all the Right Stuff out of the Right Heart Catheter | Ioannis Mastoris, MD |
9:15 | Critical Care Echocardiography and Ultrasonography | Jona Ludmir, MD, & Aranya Bagchi, MD |
9:35 | Panel Discussion: Tools of the Trade |
9:55 | BREAK |
Section II: Initial Entry and Management of Cardiac Critical Care Patients | |
10:05 | Acute Myocardial Infraction – Cardiogenic Shock | Marc Sabatine, MD |
10:25 | Cardiac Arrest: Evidence-based Management | Michael Silverman, MD, MPH |
10:40 | Cardiopulmonary Bypass and Postoperative Monitoring and Management | |
10:55 | Critical Care of Post-Transcatheter Therapy Patients and Acute Valvular Emergencies | |
11:10 | Panel Discussion: Initial Entry of Cardiac Critical Care Patient |
| 11:30 | LUNCH |
Section III: Critical Heart and Lung Interactions in Cardiac Critical Care Patients | |
12:00pm | Invasive and Non-invasive Ventilation in the Cardiac Critical Care Unit: ARDS and Refractory Hypoxemia in Cardiac Disease | Kathryn Hibbert, MD |
12:15 | Cor Pulmonale and Ventricular Interdependence: Optimizing RV and LV Interactions at the Bedside | |
12:30 | Pulmonary Hypertension and Pulmonary Embolism for the Cardiac Intensivist | |
12:45 | Mastering VV and VA ECMO | Jerome Crowley, MD, MPH |
1:00 | Mobile ECMO: Strategies, Best Practices | Aaron Aguirre, MD |
1:15 | Panel Discussion: Critical Heart and Lung Interactions in Critical Care |
1:35 | BREAK |
Section IV: Acute and Chronic Cardiac Failure; Heart Replacement Therapies | |
| 1:45 | Cardiogenic Shock: Hub-and-Spoke Network Perspective and Optimal Practice for Transfers | Sohah Iqbal, MD |
| 2:00 | Percutaneous VAD and MCS: Overview and Indications | Ivana Nikolic, MD |
2:15 | Heart Transplant: Indications, Evaluation, and Surgery | Lana Tsao, MD |
2:30 | Critical Care of the Immediate post-VAD and post-Transplant Patient | |
2:45 | Alarm! MCS Device Emergencies | David Convissar, MD |
3:00 | Panel Discussion: Acute and Chronic Cardiac Failure; Heart Replacement Therapies |
3:20 | BREAK |
Section V: Case Records of the MGH Heart Center ICU | |
| 3:30 | Clinicopathologic Conference: Case Records of the MGH Heart Center ICU | David M. Dudzinski, MD; Mary Norine Walsh, MD; Christopher Newton-Cheh, MD, MPH; Malavika Prabhu, MD; Kyle Devins; Ina Ly, MD; Ryan Chung, MD |
| 4:30pm | Adjourn |
Saturday, April 29, 2023 | 7:50am - 12:15pm
7:50 | Welcome Back – Day 2 | David Dudzinski, JD, MD & Ivana Nikolic, MD |
| Section VI: Cardiovascular Comorbidities in the Cardiac Critical Care Units Moderators: Ivana Nikolic, MD & David Convissar, MD | |
8:00 | Tachyarrhythmia and Bradyarrhythmia in Cardiac Critical Care | Rajeev Malhotra, MD |
8:20 | Acute Aortic Syndromes: Diagnosis and Management | Eric Isselbacher, MD |
8:40 | Vascular Complications in Cardiac Critical Care: Limb Ischemia, Mesenteric Ischemia | |
9:00 | Panel Discussion: Cardiovascular Comorbidities in the Cardiac Critical Care Units |
9:20 | BREAK |
| Section VII: Non- Cardiovascular Comorbidities in the Cardiac Critical Care Units Moderators: Jill Rackliffe, NP & Amit Bardia, MD | |
9:30 | Sepsis and ICU Infection Update | Lisa Bebell, MD |
9:45 | Acute Kidney Injury and Renal Replacement Therapy | Man Piu (Mark) Wong, MD |
10:00 | Rational Approaches to Sedation and Neurologic Management in Cardiac Critical Care | |
10:15 | Rapid Evidence Review on ICU Prophylaxis and Quality in the ICU | Amit Bardia, MD |
10:30 | Panel Discussion: Optimizing Care of Non-Cardiac Comorbidities in Cardiac Critical Care |
10:50 | BREAK |
| Section VIII: Literature Update and Clinical Cases Moderators: David M. Dudzinski, MD & Kelly Tankard, MD | |
11:00 | Top 3 Papers from 2022-2023 in Cardiac Critical Care Literature | Kelly Tankard, MD |
11:15 | Challenging Cases from the MGH Cardiac Critical Care Units | David Dudzinski, JD, MD; Van-Khue Ton, MD, PhD; Jerome Crowley, MD; Eriberto Michel, MD, Emily Zern, MD |
12:05pm | Conclusion | David Dudzinski, JD, MD; Ivana Nikolic, MD; Jill Rackliffe, NP |
| 12:10pm | Adjourn |
[format] => full_html ) [field_registration_instructions] => Array ( [value] =>
| Registration Type | Registration Fee |
|---|---|
| Physicians/Allied Heart Care Professionals | $195.00 |
| Fellows in Training | $75.00 |
Cancellation Policy:
Registrations cancelled on or before April 14, 2023 will be refunded, less a $20 administrative fee. Registrations cancelled after April 14, 2023 will not be refunded.
Contact partnerscpd@partners.org if you require assistance in cancelling your online registration.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for physicians, nurses, pharmacists, physician assistants, and other members of the healthcare team. This activity is intended for providers in the specialties of Anesthesiology, Cardiac Electrophysiology, Cardiac Surgery, Cardiology, Critical Care, Emergency Medicine, Geriatric Medicine, Internal Medicine, Interventional Cardiology, Pulmonary Disease, Thoracic Surgery, and Vascular Surgery.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/2498 [id] => 2498 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital - Corrigan Minehan Heart Center and
Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=67035
[first] => https://cpd.partners.org/node?nid=67035&page=0
[last] => https://cpd.partners.org/node?nid=67035&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this live activity for a maximum of 13.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 13.5 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/231
[id] => 231
[resource] => taxonomy_term
[uuid] => 541dec03-c6af-4bcb-9af7-8fa28fedfb53
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1695660120
[value2] => 1725076740
[duration] => 29416620
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1718366400
[value2] => 1718481600
[duration] => 115200
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/4
[id] => 4
[resource] => taxonomy_term
[uuid] => c57cf9bf-73d6-4eaa-9f35-e4e9cce75d36
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/66169
[id] => 66169
[resource] => file
[uuid] => 0dfe4e92-152c-4f86-81e9-db92e337162a
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 46161
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Mass General Brigham
[street] => 399 Revolution Drive
[additional] => Assembly Row
[city] => Somerville
[province] => MA
[postal_code] => 02145
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => THIS IS A HYBRID EVENT
Non Healthcare Professionals Registration Instructions:  Cancer Equity Colloquium 2024_registration instructions.pdf
Cancer Equity Colloquium 2024_registration instructions.pdf
Now more than ever, the presence of social inequities in healthcare is evident. This two-day, hybrid event, the Cancer Equity Colloquium, will address the diverse issues that underlie cancer inequities. The goal of the Colloquium is to bring together individuals from healthcare, academia, private/public business sector, and the public at large to develop unique approaches to tackling these inequities. We know that impactful initiatives to promote cancer equity require the skills and experiences of individuals from all these sectors of society. The speakers will reflect a similar mixture of backgrounds. Attendees will have the opportunity to engage with each other and the Cancer Equity Colloquium faculty to potentially develop novel partnerships.
| Registration Type | Registration Fee |
|---|---|
| Physician | $199.00 |
| Nurses and Other Allied Professionals | $99.00 |
| General Public | $49.00 |
| Industry | $299.00 |
COURSE CO-DIRECTORS
Colin D. Weekes, MD, PhD, FASCO
Christopher D. Horner Endowed Chair in Pancreatic Cancer,
Director, Pancreatic Cancer Research,
Director, Cancer Center Grand Rounds,
Director, Equity, Division of Hematology/Oncology,
Massachusetts General Hospital Cancer Center;
Associate Professor of Medicine, Harvard Medical School
Brenda Lormil-Raymond, MSN, FNP-C
Equity Nurse Practitioner, Phase I Research (Termeer Center), Massachusetts General Hospital Cancer Center;
Founder, Haitian American Medical Association (HAMA)
FACULTY
Brendan Abel, JD
Healthcare Policy & Advocacy Director, Johnson & Johnson;
Teaching Faculty, Harvard Medical School Center for Bioethics
Natasha Archer, MD
Physician, Dana Farber/Boston Children's Cancer and Blood Disorders Center;
Assistant Professor of Pediatrics, Harvard Medical School
Sharl Azar, MD
Medical Director, Comprehensive Sickle Cell Disease Treatment Center,
Robert K. Kraft Chair in Diversity, Equity, and Inclusion,
Massachusetts General Hospital Cancer Center
Lourdes Baezconde-Garbanati, PhD, MPH
Associate Dean of Community Initiatives, KSOM
USC Distinguished Professor of Population and Public Health Sciences
Dept. of Population and Public Health Sciences
Associate Director of Community Outreach and Engagement, USC NCCC
Director, Center for Health Equity in the Americas (CenHealth)
Norris Comprehensive Cancer Center (USC NCCC)
Keck School of Medicine (KSOM)
University of Southern California (USC)
Aditya Bardia, MD, MPH, FASCO
Professor of Medicine, Geffen School of Medicine at UCLA,
Director, Breast Oncology Program,
Assistant Chief (Translational Research), Division of Medical Oncology,
Director of Translational Research Integration
UCLA Health Jonsson Comprehensive Cancer Center
Farrah A. Belizaire
Founder, LiteWork Events, LLC
Diversity Officer, MIT Brain & Cognitive Sciences
Regina Jeanise Brown, MD
Senior Medical Director, Clinical Research Physician
Early Development, Oncology
J&J Innovative Medicine
Johnson & Johnson
Taneshia Camillo-Sheffey
Consultant, Founder & Director,
The Haute House Design Studio
MadelNcubator, Inc
Duclas M. Charles, PharmD
Founder, Black Health Connect
Chuck Christian
Cancer Thriver
Melissa B. Davis, PhD
Director, Institute of Translational Genomic Medicine (ITGM)
Professor, Department of Microbiology, Biochemistry, and Immunology
Morehouse School of Medicine
Georgia Research Alliance Distinguished Investigator
Pastor Cesar Depaz
Senior Pastor,
Hispanic Community Church of Boston
Yves M. Duroseau, MD, MPH
Chair, Emergency Medicine, Lenox Hill Hospital
President, Medical Board, Lenox Hill Hospital
Vice President, Western Region Emergency Medicine Service Line, Northwell Health
Fena Fenelon
CEO & Founder, Sofenomenal Agency Group,
Public Speaker,
Cancer Survivor (Colorectal)
Marvella E. Ford, PhD
Professor and Vice Chair of Inclusive Excellence, Department of Public Health Sciences
Associate Director of Population Science and Community Outreach and Engagement,
Hollings Cancer Center
Medical University of South Carolina
SmartState Endowed Chair, Cancer Disparities Research, South Carolina State University
Wayne Frederick, MD, MBA
Charles R. Drew Professor of Surgery,
Howard University
Jacquelyne Gaddy, MD, MSc, MSCR
Assistant Professor,
Deputy Director, Diversity Enhancement Program in Oncology,
Yale School of Medicine
Geoffrey A. Gallo
Head of State Government Affairs
AstraZeneca
James Hills
Java with Jimmy
Richard J. Lee, MD, PhD
Clinical Co-Director, The Claire and John Bertucci Center for Genitourinary Cancers
Assistant Physician, Department of Medicine
Massachusetts General Hospital Cancer Center
Lisa Lewis, MPH
Graduate Student,
Harvard Medical School, Center for Bioethics
Harvard Medical School, Department of Global Health and Social Medicine
Rev. Jean J.M. Louis
Senior Pastor, Free Pentecostal Church of God
Lady Katlyne D. Louis
Founder of Chosen Women of God & Rèspire Retreat & Restoration
Kanisha Louis Jean, MSN, FNP-BC
Nurse Practitioner, Family Medicine, CCI Health Services
Mentor, Dotson Bridge & Mentorship Program, Simmons University;
Founder & President, MelanIN Medicine, Inc.
Luckson Mathieu, MD
Senior Clinical Reviewer
FDA Division of Oncology 2
Olorunseun O. Ogunwobi, MD, PhD
Barnett Rosenberg Professor of Biochemistry and Molecular Biology,
Chairperson, Department of Biochemistry and Molecular Biology,
Michigan State University
Kenley Preval
MD/PhD Student, UMass Medical School;
Founder, Improving Academic Medicine Underrepresentation (IAMU)
Sana Raoof, MD, PhD
Resident Physician,
Memorial Sloan-Kettering Cancer Center
Kerry Reynolds, MD
Assistant Professor, Harvard Medical School;
Associate Physician, Massachusetts General Hospital Cancer Center
Clinical Director, Inpatient Oncology
Director, Severe Immunotherapy Complications Service
Natalie Sabga
Founder, The John E. Sabga Foundation
Veronica Sandoval, PhD, JD
Principal, Patient Inclusion & Health Equity
Chief Diversity Office,
Genentech, A Member of the Roche Group
Lecia Sequist, MD, MPH
Director, Cancer Early Detection and Diagnostics Program
Massachusetts General Hospital Cancer Center;
Landry Family Professor of Medicine, Harvard Medical School
Aithan Shapira, PhD, MFA
Founder, TILT;
Senior Lecture at Sloan School of Management, MIT
Cardinale Smith, MD, PhD
Chief Medical Officer, Tisch Cancer Hospital, The Mount Sinai Hospital
Vice President and Chief Quality Officer, Tisch Cancer Center, Mount Sinai Health System
Associate Director, Community Outreach and Engagement, Tisch Cancer Institute
Professor of Medicine, Division of Hematology/Medical Oncology and
Brookdale Department of Geriatrics and Palliative Medicine
Ryan Sullivan, MD
Associate Professor, Harvard Medical School;
Peter and Ann Lambertus Endowed Chair in Cancer,
Director, Center for Melanoma,
Massachusetts General Hospital Cancer Center
Erica Stringer-Reasor, MD
Associate Professor, Division of Hematology Oncology,
Vice Chair for Diversity, Equity, and Inclusion DOM,
Director, Breast Cancer Program,
O’Neal Comprehensive Cancer Center,
University of Alabama at Birmingham
J. Kevin Tucker, MD
Vice President, Education,
Mass General Brigham
Assistant Professor of Medicine, Harvard Medical School
Katia Vincent
Spoken Word Artist
Sickle Cell Thriver
Clayton C. Yates, PhD
John R. Lewis Professor of Pathology,
Professor of Pathology, Oncology, Urologic-Oncology,
Director for Translational Health Disparities and Global Health Equity Research,
Program Co-Leader for Cancer Genetics and Epigenetics,
Sidney Kimmel Comprehensive Cancer Center,
Johns Hopkins School of Medicine
ACCOMODATIONS
A limited number of rooms have been blocked at the following nearby hotels for the nights of June 13, 14, and 15. Please see below for booking information.
Fairfield Inn Boston Medford
Click here to: Book your group rate at the Fairfield Inn Boston Medford
Room Rate: $249/night
Last Day to Book: Tuesday, May 14, 2024
AC Hotel Boston North
Click here to: Book your group rate for AC Hotel Boston North
Room Rate: $269/night
Last Day to Book: Tuesday, May 14, 2024
Other hotels in the area:
Please note we do not have a room block for either of the following hotels:
The Row Hotel at Assembly Row
La Quinta Inn & Suites
TRANSPORTATION & PARKING
The meeting venue is accessible via the Assembly Row stop on the Orange Line and MBTA Route 90 Bus from Davis Square. Additionally, there are transportation resources available through Assembly Connect. Assembly Connect programs are free for residents, employees, and visitors to the Assembly Square District of Somerville, MA.
If you choose to drive and park at the MGB Assembly Row parking garage where the event is being held, the parking fees are as follows:
| Rates | |
|---|---|
| 0-3 Hours | FREE |
| 3-4 Hours | $3.00 |
| 4-5 Hours | $5.00 |
| 5-6 Hours | $15.00 |
| 6+ Hours | $27.00 |
[format] => full_html ) [field_hotel_link] => Array ( ) [field_hotel_photo] => Array ( ) [field_hotel_travel] => Array ( ) [field_learning_objectives] => Array ( [value] =>
Upon completion of this activity, participants will be able to:
- Recognize the determinants that drive cancer care inequity.
- Formulate solutions to address factors leading to cancer inequity.
- Develop collaborative initiatives to promote equity in cancer care.
- Demonstrate the role of team science in the improvement of cancer inequities.
Promotional Supporters
For more information, please contact ebrooks3@mgb.org
![]() Cancer Equity Colloquium 2024_Promotional Supporters.pdf
Cancer Equity Colloquium 2024_Promotional Supporters.pdf
FUNDING
Cancer Equity Colloquium 2024 has received support in the form of an educational grant from the following companies:
Astellas Pharma Global Development, Inc.
Bristol Myers Squibb
Merck Sharp & Dohme LLC
Sun Pharma
[format] => full_html ) [field_program] => Array ( [value] =>
Friday, June 14, 2024 | 7:15am - 5:00pm
| 7:15am | Registration and Breakfast* |
| 8:00 | Introduction | Colin D. Weekes, MD, PhD & Brenda Lormil-Raymond, MSN, FNP-C |
| 8:10 | Keynote Address | Wayne Frederick, MD, MBA |
| 8:45 | Clinical Trial Diversification | Moderator: Colin D. Weekes, MD, PhD Panelists: Luckson Mathieu, MD; Regina Jeanise Brown, MD; Erica Stringer-Reasor, MD |
| 9:45 | Intentional Engagement Session |
| 10:00 | BREAK* |
| 10:05 | The Evolving Therapeutic Paradigm for Sickle Cell Disease: Food for Thought Moderator: Katia Vincent Panelists: Natasha Archer, MD; Sharl Azar, MD; Yves M. Duroseau, MD, MPH |
| 10:55 | Cancer From My Lens Moderator: Taneisha Camillo-Sheffy Panelists: Chuck Christian; Fena Fenelon; Natalie Sabga; J. Kevin Tucker, MD |
| 11:55 | LUNCH* |
| 12:30pm | Cancer Immunotherapy Moderator: Richard J. Lee, MD, PhD Panelists: Ryan Sullivan, MD & Kerry Reynolds, MD |
| 1:30 | Cancer Screening Redefined | Sana Raoof, MD, PhD |
| 2:00 | BREAK* |
| 2:15 | Disease-Specific Breakout Sessions: Breast | Aditya Bardia, MD, MPH, FASCO & Melissa B. Davis, PhD Colon | Jacquelyne Gaddy, MD, MSc, MSCR & Olorunseun O. Ogunwobi, MD, PhD Prostate | Richard J. Lee, MD, PhD & Clayton Yates, PhD Lung | Lecia Sequist, MD, MPH & Cardinale Smith, MD, PhD |
| 4:00 | Intentional Engagement Session |
| 4:15 | A Year in Review Moderator: Pastor Cesar Depaz Panelists: Rev. Jean J.M. Louis & Lady Katlyne D. Louis |
| 4:45 | Wrap-Up |
| 5:00pm | Adjourn |
5:00 - 7:00pm – Welcome Reception
*The exhibit hall will be open during breakfast, breaks, and lunch
Saturday, June 15, 2024 | 8:30am - 4:00pm
| 8:30am | Breakfast* |
| 9:00 | Welcome | Colin D. Weekes, MD, PhD & Brenda Lormil-Raymond, MSN, FNP-C |
| 9:05 | Leadership: Catalysts for Transformation | Aithan Shapira, PhD, MFA |
| 9:40 | Unique Scientific Approaches to Cancer Genomics | Melissa B. Davis, PhD & Clayton Yates, PhD |
| 10:30 | Intentional Engagement Session |
| 10:45 | The Power of Community Networking | |
| 11:45 | Cultivating the Next Generation | Kenley M. Preval |
| 12:10 | LUNCH* & Fireside Chat | Wayne Frederick, MD, MBA & Colin D. Weekes, MD, PhD |
| 1:00 | Innovative Approaches to Building Community & Academic Partnerships | Moderator: Aditya Bardia, MD, MPH, FASCO Panelists: Lourdes Baezconde-Garbanati, PhD, MPH; Marvella E. Ford, PhD; Cardinale Smith, MD, PhD |
| 2:00 | BREAK* |
| 2:10 | Activating Advocacy Through Policy Moderator: Lisa Lewis, MPH Panelists: Veronica Sandoval, PhD, JD; Brenda Abel, JD; Geoffrey A. Gallo |
| 3:10 | Fireside Chat | Aithan Shapira, PhD, MFA & Colin D. Weekes, MD, PhD |
| 3:55 | Closing Remarks |
| 4:00pm | Adjourn |
*The exhibit hall will be open during breakfast, breaks, and lunch
| Registration Type | Registration Fee |
|---|---|
| Physician | $199.00 |
| Nurses and Other Allied Professionals | $99.00 |
| General Public | $49.00 |
| Industry | $299.00 |
Cancellation Policy:
Registrations cancelled on or before May 31, 2024 will be refunded, less a $20 administrative fee. Registrations cancelled after May 31, 2024 will not be refunded.
Contact partnerscpd@partners.org if you require assistance in cancelling your online registration.
ACCOMODATIONS/TRAVEL
A limited number of rooms have been blocked at the following nearby hotels for the nights of June 13, 14, and 15. Please see below for booking information.
Fairfield Inn Boston Medford
Click here to: Book your group rate at the Fairfield Inn Boston Medford
Room Rate: $249/night
Last Day to Book: Tuesday, May 14, 2024
AC Hotel Boston North
Click here to: Book your group rate for AC Hotel Boston North
Room Rate: $269/night
Last Day to Book: Tuesday, May 14, 2024
Other hotels in the area:
Please note we do not have a room block for either of the following hotels:
The Row Hotel at Assembly Row
La Quinta Inn & Suites
TRANSPORTATION & PARKING
The meeting venue is accessible via the Assembly Row stop on the Orange Line and MBTA Route 90 Bus from Davis Square. Additionally, there are transportation resources available through Assembly Connect. Assembly Connect programs are free for residents, employees, and visitors to the Assembly Square District of Somerville, MA.
If you choose to drive and park at the MGB Assembly Row parking garage where the event is being held, the parking fees are as follows:
| Rates | |
|---|---|
| 0-3 Hours | FREE |
| 3-4 Hours | $3.00 |
| 4-5 Hours | $5.00 |
| 5-6 Hours | $15.00 |
| 6+ Hours | $27.00 |
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>
This activity is intended for Physicians, Nurses, Pharmacists, Psychologists, Physician Assistants, Social Workers, Other members of the healthcare team, General Public, and Patients & Caregivers.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3008 [id] => 3008 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital Cancer Center & Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=42677
[first] => https://cpd.partners.org/node?nid=42677&page=0
[last] => https://cpd.partners.org/node?nid=42677&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this live activity for a maximum of 5 AMA PRA Category 1 CreditsTM. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 5 Nursing contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
Physician Assistants
Mass General Brigham has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 1 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation.

Psychologists
5 Continuing Education (CE) credits are awarded
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/228
[id] => 228
[resource] => taxonomy_term
[uuid] => 46179069-8cd4-41d6-9576-43b10dc11784
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1649332800
[value2] => 1676350740
[duration] => 27017940
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1663340400
[value2] => 1673629200
[duration] => 10288800
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/238
[id] => 238
[resource] => taxonomy_term
[uuid] => fd81c17a-d19b-46b8-ad6b-2c5aee9ce9be
)
[1] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/239
[id] => 239
[resource] => taxonomy_term
[uuid] => 8fe8f562-9596-41a9-8e2f-c93aa2c8dae9
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/42067
[id] => 42067
[resource] => file
[uuid] => 088328a5-b9b4-4bb2-bc37-95c26183fa13
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 25571
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Mass General Brigham
[street] =>
[additional] =>
[city] => Somerville
[province] => MA
[postal_code] =>
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => This event will take place virtually, via Zoom.
Details provided upon registration
Description
Mass General Brigham’s Virtual Care Speaker Series, led by our industry's most widely regarded stakeholders, thought leaders and policy experts, will feature a deep-dive into the evolving virtual care landscape and dig into how to build and optimize virtual care programs as a permanent modality in care delivery. Dynamic panels will lead in-depth discussions about advancing the reach of virtual and hybrid patient care at a critical time for hospitals and health care.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Course Director
Lee Schwamm, MD
Vice President, Virtual Care,
Mass General Brigham

Dr. Schwamm is Professor of Neurology at Harvard Medical School and holds the C. Miller Fisher Chair in Vascular Neurology at MGH, where he serves as the Senior Clinical and Strategic Advisor to the Dept of Neurology and Director of the Center for TeleHealth. He leads all systemwide virtual care (telehealth) activities for the Mass General Brigham Health System as Vice President of Digital Patient Experience/Virtual Care (synchronous and synchronous virtual visits and consults, remote patient monitoring, virtual urgent care and online second opinions). During COVID, he led adoption efforts for 10,000 providers and 1.38 M visits, and introduced a suite of inpatient virtual solutions. He has spent 2 decades in telehealth, pioneering telestroke and leading advocacy efforts (e.g., FAST Act in Congress). He is a an internationally recognized expert in stroke diagnosis, treatment and prevention and a Fellow of the American Heart Association and American Neurological Association. He is the author of >450 peer-reviewed articles and has chaired many of the current practice guidelines for stroke and telehealth-enabled care delivery. He has received numerous awards for innovation, leadership and advocacy in the field of stroke and digital health. He serves as the section editor for digital health for Stroke, and on the international advisory board for Lancet Digital Health. His research has been funded by NIH, PCORI, AHRQ, HRSA, CDC, and others. He serves on the Board of Directors of the American Heart Association.
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
[value] => This event will take place virtually, via Zoom. Details provided upon registration
[format] => full_html
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this course, participants will be able to:
- Create, enhance, and extend the virtual care blueprint at their institution.
- Apply best practices, interpersonal bedside skills, and multidisciplinary approaches to improve your virtual patient experience.
- Identify necessary technology tools needed to successfully provide industry-leading virtual care services.
- Integrate existing platforms in the virtual care space.
- Demonstrate how to operationalize and engage with virtual care.
ABIM MOC Information
- Maintenance of Certification (MOC) points can only be awarded if you attended the entire hour session.
- Upon successful completion of this activity, if you wish to receive MOC II points you will need to enter your ABIM ID number, and Date of Birth (mm/dd) at the beginning of the evaluation.
- The Mass General Brigham Office of Continuing Professional Development will verify completion of this activity and report to the ABIM.
- Diplomates must check their ABIM Portfolio for confirmation of your MOC II points.
MOC Recognition Statement
Successful completion of this CME activity, which includes participation in the activity, with individual assessments of the participant and feedback to the participant, enables the participant to earn 1 MOC point in the American Board of Internal Medicine (ABIM) Maintenance of Certification (MOC) program. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
[format] => full_html ) [field_program] => Array ( [value] =>
September 16, 2022
11:00am - 12:00pm ET
Session 1: Keeping Pace with Rapid Change: The Virtual Care Revolution
Virtual care has undoubtedly reshaped the future of health care. With a rapid growth in consumer expectations and consumption of virtual options from both patients and providers, we explore how the virtual care experience can be optimized as health care undergoes digital transformation. This session will delve into the history of virtual care, the current landscape and rapid expansion of emerging technologies expanding the reach of care.
Session Format: Didactic Lecture
Speaker
Lee Schwamm, MD
Vice President, Virtual Care,
Mass General Brigham
October 14, 2022
11:00am - 12:00pm ET
Session 2: Pushing the Arc Towards “Techquity”: Patient-Centric Virtual Care
Join patient experience experts in discussing ways to bring health equity in virtual care to the next level for patients. Experts will analyze interdisciplinary approaches to improve patient satisfaction. COVID exacerbated the preexisting inequities in care for vulnerable populations, and while virtual care restored access to care for many, in some cases it further deepened these disparities. This session will focus on the interaction between health equity, digital health and the patient experience, and how health systems can design for these challenges.
Session Format: Panel Discussion
Moderator
Lee Park, MD, MPH
Instructor in Medicine, Harvard Medical School;
Internist, Brigham and Women's Hospital;
Senior Medical Director, QPE Digital Health,
Quality and Patient Experience, Mass General Brigham
Speakers
Esteban Barreto, PhD
Director, Evaluation of Equity and Community Health,
Massachusetts General Hospital
Allison Bryant Mantha, MD, MPH
Associate Professor of Obstetrics, Gynecology and Reproductive Sciences,
Harvard Medical School;
Maternal-Fetal Medicine Specialist,
Frederic D. Frigoletto, MD Endowed Chair,
Department of Obstetrics and Gynecology,
Massachusetts General Hospital;
Senior Medical Director for Health Equity, Mass General Brigham
Dan Noyes
Co-CEO, Tech Goes Home
Aswita Tan-McGrory, MBA, MSPH
Adjunct Faculty, Northeastern University;
Director, the Disparities Solutions Center,
Director, Equity in Care Implementation,
Administrative Director of Research, Department of Medicine,
Massachusetts General Hospital
November 10, 2022
11:00am - 12:00pm ET
Session 3: The Human Experience of the Digital Patient
As virtual care has rapidly expanded; the role of telepresence is here to stay. This session will discuss the importance of developing a trust-based relationship between patient and provider to increase overall patient satisfaction and better health outcomes. Stakeholders will provide insights on how to foster a comfortable setting for the patient and how to upgrade their “webside” manner.
Session Format: Simulation and Panel Discussion
Moderator
Lydia C Siegel, MD, MPH
Internal Medicine, Brigham and Women’s Hospital;
Medical Director, Ambulatory Services in Clinical Informatics,
Mass General Brigham
Panelists
Oscar Benavidez, MD
Chief, Division of Pediatric Cardiology,
Massachusetts General Hospital
David Binder, MD
Medical Director, Spaulding Outpatient,
Spaulding Rehabilitation Network
Susan Edgman-Levitan, PA
Associate in Health Policy, Harvard Medical School;
Executive Director, John D. Stoeckle Center for Primary Care Innovation,
Massachusetts General Hospital
Darlene Sawicki, MSN, NP-BC
Director of Advanced Practice Providers,
Massachusetts General Hospital
Shyam K. Tanguturi, MD
Radiation Oncology,
Dana-Farber Cancer Institute
December 9, 2022
11:00am - 12:00pm ET
Session 4: Watch your Tech: Leveraging Technology for Care
In an era where Virtual Care is a core component of how care is delivered and will continue to grow as a core part of our healthcare system, designing and deploying technology solutions for providers and patients to use is critical. This session will cover intuitive Virtual Care deployment and how to provide existing virtual-based technologies for digital solutions. Experts will review strategies to increase technology adoption at their institution and provide demos of MGB-developed platforms that are currently in use at the bedside.
Session Format: Demo and Panel Discussion
Moderator
Adam Landman, MD, MS, MIS, MHS
Senior Vice President, Digital
Chief Information Officer,
Mass General Brigham
Panel
Anne Bane, MSN, RN, BC
Nurse Director, Nursing Informatics and Medication Safety,
Center for Nursing Excellence,
Brigham and Women's Hospital
Mike Carter
Program Director, Health Information Systems,
Mass General Brigham
Juan Estrada
Senior Director, Center for TeleHealth,
Massachusetts General Hospital
Benji Meller
Program Director, Technology Operations and Inpatient Virtual Care,
Massachusetts General Hospital
Daniel Meninger, MSPT, MBA
Program Manager, Virtual Care Services,
Spaulding Rehabilitation Network
Radhika Sangireddy
Virtual Care Portfolio Manager,
Mass General Brigham
Mark Zhang, DO, MMSc
Medical Director, Brigham Digital Innovation Hub,
Medical Director, Digital Health Implementation,
Brigham and Women’s Hospital
January 13, 2023
11:00am - 12:00pm ET
Session 5: The Rules of the Virtual Road: The Regulatory Landscape of Telehealth
Health care systems are increasing their use of virtual care in the setting of technology that is evolving at the speed of light. As a result, the regulatory and legal landscape in virtual care is constantly evolving. This expert panel will provide real-life examples from care settings and analyze state and federal regulations that govern the provision of virtual care.
Session Format: Simulation and Panel Discussion
Moderators
Kate Connelly, CPA, MBA
Corporate Director, Enterprise Risk Management,
Mass General Brigham
Rosemary Gottlieb
Senior Legal Counsel,
Office of the General Counsel,
Mass General Brigham
Panelists
Lindsey Reilly
Director, Billing Compliance,
Brigham and Women’s Hospital
Massachusetts General Hospital
Marcy Simoni, MPH
Mass General Brigham
Tim Willens, MD
Chief, Division of Child and Adolescent Psychiatry,
Co-Director for Center for Addiction Medicine,
Massachusetts General Hospital
Alexis Williamson, MPH
Executive Director of Central Credentialing,
Mass General Brigham
[format] => full_html ) [field_registration_instructions] => Array ( ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>
This program is recommended for virtual care providers, healthcare professionals and organizations seeking to fine tune, develop or launch their Virtual Care programs.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/1862 [id] => 1862 [resource] => accme_data ) [field_show_on_calendar] => [field_custom_provided] => Array ( [value] =>Mass General Brigham, Virtual Care &
Mass General Brigham's Office of Continuing Professional Development
Array
(
[self] => https://cpd.partners.org/node?nid=59046
[first] => https://cpd.partners.org/node?nid=59046&page=0
[last] => https://cpd.partners.org/node?nid=59046&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 Credits™
Mass General Brigham designates this live activity for a maximum of 8 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 8 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
Physician Assistants
Mass General Brigham has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 8 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation.

MOC Recognition Statement
Successful completion of this CME activity, which includes participation in the activity, with individual assessments of the participant and feedback to the participant, enables the participant to earn 8 MOC points in the American Board of Internal Medicine (ABIM) Maintenance of Certification (MOC) program. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/197
[id] => 197
[resource] => taxonomy_term
[uuid] => 621a8034-627c-4c33-b273-260b2d83768c
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1687793400
[value2] => 1706763540
[duration] => 18970140
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1701435000
[value2] => 1701468000
[duration] => 33000
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/7
[id] => 7
[resource] => taxonomy_term
[uuid] => 2a38b69f-4c76-44b0-bde5-67e901205c53
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/52190
[id] => 52190
[resource] => file
[uuid] => f6427650-3a3b-4050-bb7b-0c660ba2c578
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 44291
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Livestream
[street] => Massachusetts General Hospital
[additional] =>
[city] => Boston
[province] => MA
[postal_code] => 02114
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => This is a virtual course
December 1, 2023

This course provides education on acute and chronic aortic conditions to physicians and APPs who might encounter patients with these conditions in their practice but may not have sufficient familiarity with their management. The course will have two sessions – morning and afternoon. The morning session will focus on the fundamentals of aortic aneurysms and chronic aortic disease and will be targeted to PCPs, cardiologists and APPs. The afternoon session will focus on aortic dissection and other acute aortic syndromes, which will be more relevant to ER physicians and APPs.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Course Directors
Arminder Jassar, MBBS

Cardiac Surgeon, Massachusetts General Hospital;
Assistant Professor of Surgery, Harvard Medical School
Matt Eagleton, MD

Chief of Division of Vascular and Endovascular Surgery, Massachusetts General Hospital;
Professor of Surgery in the Field of Vascular and Endovascular Surgery, Harvard Medical School
Eric Isselbacher, MD, MSc

Cardiologist, Massachusetts General Hospital;
Associate Professor of Medicine, Harvard Medical School
Faculty
Jordan Bloom MD, MPH

Cardiac Surgeon, Massachusetts General Hospital;
Assistant Professor of Surgery, Harvard Medical School
Duke Cameron, MD
Cardio-Thoracic Surgeon and Co-Director of the Marfan Syndrome and Related Conditions Clinic,
Massachusetts General Hospital
Jared Conley, MD, PhD, MPH

Emergency Medicine, Massachusetts General Hospital;
Assistant Professor of Emergency Medicine, Harvard Medical School
Anahita Dua, MD, MS, MBA

Vascular Surgeon, Massachusetts General Hospital;
Associate Professor of Surgery, Harvard Medical School
Michael Frakes, APRN, FCCM, FAEN, FACHE
Chief Quality Officer, Director of Clinical Care, Boston MedFlight
Sandeep Hedgire, MD

Radiologist, Massachusetts General Hospital;
Assistant Professor of Radiology, Harvard Medical School
Motahar Hosseini, MD

Cardiac Surgeon, Massachusetts General Hospital
Mark Lindsay, MD, PhD

Cardiologist, Pediatric Cardiologist, Massachusetts General Hospital;
Associate Professor of Medicine, Harvard Medical School
Jahan Mohebali, MD, MPH

Vascular Surgeon, Massachusetts General Hospital;
Assistant Professor of Surgery, Harvard Medical School
Phillip Rice Jr., MD

Chair of Emergency Medicine, Mass General Brigham;
Lecturer of Emergency Medicine, Harvard Medical School
Amy Spooner, MD

Cardiologist, Massachusetts General Hospital;
Instructor of Medicine, Harvard Medical School
Sunita Srivastava, MD

Vascular Surgeon, Massachusetts General Hospital;
Assistant Professor of Surgery, Harvard Medical School
Thoralf Sundt, MD

Chief, Division of Cardiac Surgery, Co-Director of the Corrigan Minehan Heart Center, Massachusetts General Hospital;
Professor of Surgery, Harvard Medical School
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Diagnose etiology, genetics and diagnosis of aortic aneurysms.
- Identify indications for surgery and understand surgical techniques involved in aneurysm treatment.
- Identify aortic dissection and other acute aortovascular syndromes.
- Improve management and surveillance of patients with aortic disease.
- Develop strategies to improve cohesive teamwork.
Social Media
Twitter:
Mass General Brigham Professional Development
@MassGenBrighCPD
MGH Corrigan Minehan Heart Center
@MGHHeartHealth
LinkedIn:
Mass General Brigham Professional Development
[format] => full_html
)
[field_program] => Array
(
[value] => | 7:55am | Welcome and Introduction | Arminder Jassar, MBBS; Eric Isselbacher, MD; Matthew Eagleton, MD |
Section I: Ascending Aortic AneurysmsArminder Jassar, MBBS & Eric Isselbacher, MD | |
8:00 | Who gets aneurysms of the proximal aorta and what do we do about them? Lessons from the 2022 Guidelines | Eric Isselbacher, MD |
8:25 | The importance of medical management of aortic aneurysms, both pre-op and post-op | Amy Spooner, MD |
8:40 | Imaging of the Aorta: Which Modality to Choose, How to Interpret Reports? | Sandeep Hedgire, MD |
9:00 | Genetics of Aortic Disease: Who to Screen, How to Screen, and When? | Mark Lindsay, MD, PhD |
9:20 | BREAK |
9:30 | Bicuspid aortic valve disease and related aortopathy; A common clinical Conundrum | Jordan Bloom MD, MPH |
| 9:50 | Surgery for the Aortic Root / Ascending Aorta and the Aortic Arch: What is going on inside the surgeon’s head? | Duke Cameron, MD |
| 10:10 | Panel Discussion and Q&A: Ascending Aortic Aneurysms | Moderators: Eric Isselbacher, MD & Arminder Jassar, MBBS Panel: Duke Cameron, MD; Jordan Bloom, MD, MPH; Mark Lindsay, MD, PhD; Sandeep Hedgire, MD; Thoralf Sundt, MD |
| 10:30 | BREAK |
Section II: Descending Aortic and Thoracoabdominal Aortic AneurysmsModerators: Duke Cameron, MD & Matthew Eagleton, MD | |
10:40 | Aortic guidelines: When to intervene on the descending and the thoracoabdominal Aorta? | Eric Isselbacher, MD |
10:50 | Open and endovascular Strategies for Descending Aortic and Thoracoabdominal Aortic Aneurysms (TAAA): Who is a candidate for what? | Matthew Eagleton, MD |
11:10 | Management of Abdominal Aortic Aneurysms in the current era: When and how? | Sunita Srivastava, MD |
11:30 | Panel Discussion and Q&A: Descending Aortic and Thoracoabdominal Aortic Aneurysms | Moderators: Duke Cameron, MD & Matthew Eagleton, MD Panel: Eric Isselbacher, MD; Sunita Srivastava, MD; Amy Spooner, MD, MPH |
| 11:50 | Lunch Break |
Session III: Aortic Dissection and other Acute Aortic SyndromesModerators: Jared Conley, MD, PhD, MPH and Arminder Jassar, MBBS | |
12:30 | The most lethal aortic complication: Overview of Acute aortic dissection | Jahan Mohebali, MD, MPH |
12:50 | Does my patient have an aortic dissection? | Jared Conley, MD, PhD, MPH |
1:10 | My patient has an Aortic Dissection – what else should I look for? | Arminder Jassar, MBBS |
1:30 | Waiting for transfer – what can I do? Initial Management, Lines, and Drugs | Phillip Rice Jr., MD |
1:50 | Pack your Bags, Ready for Transfer | Michael Frakes, APRN, FCCM, FAEN, FACHE |
2:10 | Panel Discussion and Q&A | Moderators: Jared Conley, MD, PhD, MPH & Arminder Jassar, MBBS Panel: Eric Isselbacher, MD; Phillip Rice Jr., MD; Michael Frakes, APRN, FCCM, FAEN, FACHE; Jahan Mohebali MD, MPH |
| 2:35 | BREAK |
Session IV: Aortic Dissection and other Acute Aortic Syndromes IIModerators: Matthew Eagleton, MD & Eric Isselbacher, MD | |
2:50 | The patient left my ER – I wonder what is happening to them now? | Arminder Jassar, MBBS |
3:10 | Surgery for Acute Type A Aortic Dissection: One Size Fits All | Thor Sundt, MD |
3:30 | Acute Type B Dissections: when to intervene? | Jahan Mohebali, MD, MPH |
3:50 | Ruptured Abdominal Aortic Aneurysm: From ER to OR | Anahita Dua, MD, MS, MBA |
| 4:10 | Lifetime management of aortic dissection: surveillance after initial repair | Motahar Hosseini, MD |
4:30 | Panel Discussion and Q&A | Moderator: Matt Eagleton, MD & Eric Isselbacher, MD Panel: Thor Sundt, MD, Jahan Mohebali, MD, MPH, Anahita Dua, MD, MS, MBA; Arminder Jassar, MBBS; Motahar Hosseini, MD |
4:55 | Conclusion | Arminder Jassar, MBBS; Eric Isselbacher, MD; Matthew Eagleton, MD |
| 5:00pm | Adjourn |
[format] => full_html ) [field_registration_instructions] => Array ( [value] =>
| Registration Type | Early Bird Rate (Before November 1, 2023) | Standard Rate (After November 1, 2023) |
|---|---|---|
| Physicians | $100.00 | $125.00 |
| Allied Health Care Professionals | $100.00 | $125.00 |
| Residents/Fellows | $50.00 | $50.00 |
Cancellation Policy:
Registrations cancelled on or before November 17, 2023 will be refunded, less a $15 administrative fee. Registrations cancelled after November 17, 2023 will not be refunded.
Contact partnerscpd@partners.org if you require assistance in cancelling your online registration.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for Physicians, Nurses, Physician Assistants in the following specialties Cardiology, Critical Care, Emergency Medicine, General Practice, Geriatric Medicine, Hematology/Oncology, Internal Medicine, Interventional Cardiology, Obstetrics/Gynecology, Peripheral Vascular Disease, Primary Care, Pulmonary Disease, and Sports Medicine.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/2800 [id] => 2800 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital - Corrigan Minehan Heart Center and
Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=70300
[first] => https://cpd.partners.org/node?nid=70300&page=0
[last] => https://cpd.partners.org/node?nid=70300&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this live activity for a maximum of 7.25 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 7.25 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/244
[id] => 244
[resource] => taxonomy_term
[uuid] => 41b0f6bc-954e-439d-b355-009eb871e393
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1711117920
[value2] => 1733115540
[duration] => 21997620
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1730461200
[value2] => 1730492100
[duration] => 30900
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/238
[id] => 238
[resource] => taxonomy_term
[uuid] => fd81c17a-d19b-46b8-ad6b-2c5aee9ce9be
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/65498
[id] => 65498
[resource] => file
[uuid] => db9870c9-3bb9-4265-9777-af151f9ebede
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 50661
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Joseph B. Martin Conference Center
[street] => 77 Avenue Louis Pasteur
[additional] =>
[city] => Boston
[province] => MA
[postal_code] => 02115
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => This is a Hybrid Course
Staying abreast of the rapidly advancing field of prostate imaging is paramount to the successful staging and treatment of patients with prostate cancer. This one-day CME course, State of the Art Imaging in the Diagnosis and Management of Prostate Cancer, will discuss current and new developments in multiparametric MRI (mpMRI), MRI-ultrasound fusion biopsy, including transperineal biopsy, PSMA PET imaging, focal therapy treatment options, and other recent advances in imaging technology and diagnostics/therapeutics for prostate cancer. The course is designed to provide a focused, yet comprehensive advanced clinical review for practicing urologists, radiologists, medical oncologists, and radiation oncologists, as well as advanced practice providers. Participant learning and interaction will be encouraged through case reviews, question-and-answer sessions, and interaction with the course faculty.
| Registration Type | Tuition Fee |
|---|---|
| In-Person | $250.00 |
| Virtual | $200.00 |
[summary] => [format] => full_html ) [field_course_transcript] => 1 [field_enrollment_requirement_min] => [field_enrollment_requirements] => Array ( ) [field_faculty_credentials] => Array ( [value] =>
Course Directors
Adam S. Feldman, MD, MPH
Massachusetts General Hospital Cancer Center
Mukesh Harisinghani, MD
Massachusetts General Hospital
Faculty
Rory Cochran, MD, PhD
Massachusetts General Hospital
Alexander Cole, MD
Brigham and Women’s Hospital
Douglas Dahl, MD
Massachusetts General Hospital
Jason Efstathiou, MD, DPhil
Massachusetts General Hospital
Sophia Kamran, MD
Massachusetts General Hospital
Adam Kibel, MD
Brigham and Women’s Hospital
Richard J. Lee, MD
Massachusetts General Hospital Cancer Center
Avinash Maganty, MD
Massachusetts General Hospital Cancer Center
Keyan Salari, MD, PhD
Massachusetts General Hospital
Philip Saylor, MD
Massachusetts General Hospital Cancer Center
Minhaj Siddiqui, MD
Salem Hospital
Baris Turkbey, MD
National Institute of Health
Robert Wang, MD
Massachusetts General Hospital
Matthew Wszolek, MD
Massachusetts General Hospital
Anthony Zietman, MD
Massachusetts General Hospital
Upon completion of this activity, participants will be able to:
- Define the most up-to-date imaging evaluation of patients with localized and advanced prostate cancer.
- Assess upcoming novel imaging techniques for the evaluation of prostate cancer.
- Describe imaging-based diagnostic and therapeutic procedural modalities including fusion biopsy and focal therapy.
- Apply the most current state-of-the-art mpMRI imaging in the care of prostate cancer patients or those with a suspicion of prostate cancer.
- Develop strategies for the healthcare team to incorporate MRI-ultrasound fusion prostate biopsy in clinical practice.
- Integrate the most current pathophysiological and pathological concepts into the interpretation of mpMRI.
FOR EXHIBIT SPACE, PLEASE CONTACT EBROOKS3@MGB.ORG
![]() State of the Art Imaging in the Diagnosis and Management of Prostate Cancer_Exhibitors.pdf
State of the Art Imaging in the Diagnosis and Management of Prostate Cancer_Exhibitors.pdf
[format] => full_html ) [field_program] => Array ( [value] =>
| 7:00am | Registration and Breakfast |
| 7:40 | Introduction and Welcome | Adam S. Feldman, MD, MPH & Mukesh Harisinghani, MD |
Session 1: Imaging of the Prostate for Diagnosis | |
| 7:45 | Multiparametric MRI – Current State of the Art and Future Directions | Mukesh Harisinghani, MD |
| 8:15 | MRI in the Patient with an Elevated PSA – Standard of Care | Robert Wang, MD |
| 8:45 | Utilization of Other Diagnostics/Biomarkers | Adam Kibel, MD |
| 9:15 | What to do After Negative Prostate MRI and Negative Fusion Biopsy | Adam Feldman, MD, MPH |
| 9:35 | Break |
Session 2: Imaging of the Prostate for Treatment | |
| 10:00 | Imaging for Staging and Treatment Planning — Surgery | Keyan Salari, MD, PhD |
| 10:30 | Imaging for Staging and Treatment Planning — Radiation | Jason Efstathiou, MD, DPhil |
| 11:00 | PSMA and Molecular Imaging of Prostate Cancer | Baris Turkbey, MD |
| 11:30 | Imaging of Advanced Disease | Philip Saylor, MD |
| 12:00pm | Lunch |
Session 3: MRI-Guided Diagnostics and Treatment | |
| 12:45 | Transperineal Prostate Biopsy | Douglas Dahl, MD |
| 1:10 | Utilization of MRI and Fusion Biopsy in the Active Surveillance Patient | Minhaj Siddiqui, MD |
| 1:35 | Utilization of Focal Therapy: When Is It Appropriate? | Alexander Cole, MD |
| 2:00 | Break |
Session 4: Case-Based Panel Discussions | |
| 2:15 | Diagnostic Dilemmas | Rory Cochran, MD, PhD; Avinash Maganty, MD; Minhaj Siddiqui, MD |
| 2:45 | The Active Surveillance Patient | Baris Turkbey, MD; Matthew Wszolek, MD; Anthony Zietman, MD |
| 3:15 | Locally Advanced Disease | Douglas Dahl, MD; Mukesh Harisinghani, MD; Sophia Kamran, MD |
| 3:45 | Metastatic Prostate Cancer | Rory Cochran, MD, PhD; Jason Efstathiou, MD, DPhil; Richard J. Lee, MD |
| 4:15pm | Thank you and Adjourn |
[format] => full_html ) [field_registration_instructions] => Array ( [value] =>
| Registration Type | Tuition Fee |
|---|---|
| In-Person | $250.00 |
| Virtual | $200.00 |
Cancellation Policy:
Registrations cancelled on or before October 18, 2024 will be refunded, less a $35 administrative fee. Registrations cancelled after October 18, 2024 will not be refunded.
Contact partnerscpd@partners.org if you require assistance in cancelling your online registration.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for physicians, nurses, physician assistants, and other members of the healthcare team.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3182 [id] => 3182 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital Cancer Center & Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=83168
[first] => https://cpd.partners.org/node?nid=83168&page=0
[last] => https://cpd.partners.org/node?nid=83168&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this live activity for a maximum of 24.25 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Physician Assistants
Mass General Brigham has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 24.25 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation.

[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/544
[id] => 544
[resource] => taxonomy_term
[uuid] => e6200947-11c0-4b3d-9d26-1b4fbf33d98e
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1737990000
[value2] => 1752379140
[duration] => 14389140
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1749474000
[value2] => 1749745800
[duration] => 271800
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/238
[id] => 238
[resource] => taxonomy_term
[uuid] => fd81c17a-d19b-46b8-ad6b-2c5aee9ce9be
)
[1] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/7
[id] => 7
[resource] => taxonomy_term
[uuid] => 2a38b69f-4c76-44b0-bde5-67e901205c53
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/80827
[id] => 80827
[resource] => file
[uuid] => 5a7241d5-891c-4767-be32-a50fa98d3178
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 58585
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Assembly Row/Live-Virtual
[street] => 399 Revolution Drive
[additional] =>
[city] => Somerville
[province] => MA
[postal_code] => 02145
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => Live-Virtual: June 9-11, 2025
Additional In-Person Live Workshop: June 12, 2025 | Mass General Brigham, Assembly Row, Somerville, MA
Neurology for the Non-Neurologist was founded by Dr. Marty Samuels 30+ years ago and we are hoping to continue his legacy for years to come! This is a comprehensive live CME course that will provide attendees with the opportunity to improve knowledge, competence, and performance in the major sub-specialty areas of modern clinical neurology. The activity will incorporate presentations, Q&A, multiple-choice questions, and opportunities for the learners to interact with experts in the field. The course will provide updates on the rapidly changing field of clinical neurology. With the knowledge and competence gained, the learner will improve their ability to skillfully diagnose and manage those patients who present with neurological symptoms and disorders.
Commercial Disclosure Statement
Neurology for the Non-Neurologist has received support in the form of an educational grant from the following companies:
EMD Serono, Inc.
Novartis Pharmaceuticals Corporation
Virtual Course + In-Person Workshop
| Tuition Type | Tuition Fee |
Physician (MD/DO) | $1000 |
Nurse (RN/APRN), Physician Assistant, Allied Health Professional/Other | $700 |
Medical Student, Resident, or Fellow (Trainee) | $300 |
Virtual Course ONLY
| Tuition Type | Early Bird Tuition Fee (ends April 7) | Regular Tuition (After April 7) |
Physician (MD/DO) | $600 | $650 |
Nurse (RN/APRN), Physician Assistant, Allied Health Professional/Other | $400 | $450 |
Medical Student, Resident, or Fellow (Trainee) | $150 | $200 |
In-Person Workshop ONLY
| Tuition Type | Tuition Fee |
Physician (MD/DO) | $500 |
Nurse (RN/APRN), Physician Assistant, Allied Health Professional/Other | $400 |
Medical Student, Resident, or Fellow (Trainee) | $150 |
Course Directors:
Galina Gheihman, MD
Assistant Professor of Neurology, Harvard Medical School;
Division of Comprehensive Neurology, Massachusetts General Hospital;
Division of General Neurology, Brigham and Women’s Hospital
Tamara B. Kaplan, MD
Assistant Professor of Neurology, Harvard Medical School;
Division of Multiple Sclerosis, Department of Neurology, Brigham and Women's Hospital
Faculty:
Kenda Alhadid-Majowski, MD, MSc., FRCPC
Instructor in Neurology, Harvard Medical School;
Adult and Pediatric Vascular Neurologist,
Massachusetts General Hospital
Denis Balaban, MD
Instructor in Neurology, Department of Neurology,
Massachusetts General Hospital
Sheena Baratono, MD
Instructor in Neurology, Harvard Medical School;
Division of Cognitive and Behavioral Neurology, Brigham and Women’s Hospital
Shamik Bhattacharyya, MD
Associate Professor of Neurology, Harvard Medical School;
Division of Spine and Spinal Cord Disorders,
Department of Neurology, Brigham and Women’s Hospital
Sarah B. Conway, MD
Instructor in Neurology, Harvard Medical School;
Divisions of Multiple Sclerosis and Hospital Neurology,
Department of Neurology, Brigham and Women’s Hospital
Emily Ferenczi, MD
Assistant Professor of Neurology, Harvard Medical School;
Division of Movement Disorders,
Department of Neurology, Mass General Brigham
Seth Gale, MD
Assistant Professor of Neurology, Harvard Medical School;
Center for Alzheimer Research and Treatment (CART),
Department of Neurology, Brigham and Women’s Hospital
Joshua P. Klein MD, PhD
Associate Professor of Neurology, Harvard Medical School;
Division of Hospital Neurology,
Department of Neurology, Brigham and Women’s Hospital
Eudocia Q. Lee, MD, MPH
Associate Professor of Neurology, Harvard Medical School;
Division of Neuro-Oncology, Brigham and Women’s Hospital/Dana Farber Cancer Institute
Jong Woo Lee, MD, MPH
Associate Professor of Neurology, Harvard Medical School;
Division of Epilepsy, Department of Neurology, Brigham and Women’s Hospital
Margaret Naclerio, MPAS, PA-C
Physician Assistant II, Department of Neurology, Brigham and Women’s Hospital
Simona Nedelcu, MD, PhD
Instructor in Neurology, Division of Stroke and Cerebrovascular Diseases,
Department of Neurology, Brigham and Women’s Hospital
Ariel Nowicki, PA-C, MS
Lead Neurosciences ICU APP, Department of Neurology, Brigham and Women’s Hospital
Meabh O’Hare, MD
Instructor in Neurology, Harvard Medical School;
Division of Neuromuscular Diseases/EMG,
Department of Neurology, Brigham and Women’s Hospital
Mary Angela O'Neal, MD
Assistant Professor of Neurology, Harvard Medical School;
Division of General Neurology,
Department of Neurology, Brigham and Women's Hospital
Claus Reinsberger, MD
Lecturer on Neurology, Harvard Medical School;
Director, Sports Neurology and Neuroscience, Mass General Brigham
Alexis Roy, MD, MSc.
Instructor in Neurology, Harvard Medical School;
Division of Stroke and Cerebrovascular Diseases,
Department of Neurology, Brigham and Women’s Hospital
Manali Sheth, MD
Instructor in Neurology, Harvard Medical School;
Division of Multiple Scherosis-Neuroimmunology,
Department of Neurology, Mass General Brigham
Samuel Snider, MD
Director, NeuroRecovery Clinic, Division of Neurocritical Care,
Brigham and Women’s Hospital;
Assistant Professor, Harvard Medical School
Angeliki Vgontzas, MD
Assistant Professor of Neurology, Harvard Medical School;
John R. Graham Headache Center, Department of Neurology,
Brigham and Women’s Faulkner Hospital
Live-Virtual: June 9-11, 2025
Additional In-Person Live Workshop: June 12, 2025 | Mass General Brigham, Assembly Row, Somerville, MA
[format] => full_html ) [field_hotel_link] => Array ( ) [field_hotel_photo] => Array ( ) [field_hotel_travel] => Array ( ) [field_learning_objectives] => Array ( [value] =>Upon completion of the activity, participants will be able to:
- Review the neurological history and approach to the neurological exam.
- Recognize how to diagnose common neurological problems such as headache, Parkinson’s disease, ischemic stroke, and dementia.
- Cite an approach to the most common neurological symptoms including headache, vision changes, weakness, dizziness, and cognitive changes.
- Apply optimal care to patients with neurological problems who do not require referral to a neurologist.
- Identify ways to provide self-management support to patients with chronic neurological conditions such as multiple sclerosis, Parkinson’s disease, or dementia.
- Recognize and manage neurological emergencies such as ischemic stroke and meningitis/encephalitis.
- Discuss the roles of members of a multi-disciplinary team, and how each contributes to optimizing outcomes for neurology patients, especially those undergoing rehabilitation or living with chronic disease (e.g. PT, OT, SLP, PM&R, etc).
Monday, June 9, 2025 | 9:00am - 4:00pm | Virtual
Fundamentals & Common Outpatient Presentations
| 9:00am | Welcome & Introduction | Galina Gheihman, MD and Tamara Kaplan, MD |
| 9:05 | Clinical Neuroanatomy for the Non-Neurologist | Galina Gheihman, MD |
| 9:45 | Test Your Knowledge | Galina Gheihman, MD; Tamara Kaplan, MD; Discussant |
| 9:55 | Q&A |
| 10:00 | The Neurological Exam for the Non-Neurologist | Tamara Kaplan, MD |
| 10:40 | Test Your Knowledge | Galina Gheihman, MD; Tamara Kaplan, MD; Discussant |
| 10:50 | Q&A |
| 10:55 | BREAK |
| 11:10 | Neuroimaging for the Non-Neurologist: What to Order and When | Joshua P. Klein, MD, PhD |
| 11:45 | Test Your Knowledge | Galina Gheihman, MD; Tamara Kaplan, MD; Discussant |
| 11:55 | Q&A |
| 12:00pm | Lunch |
| 1:00 | Headache | Angeliki Vgontzas, MD |
| 1:40 | Test Your Knowledge | Galina Gheihman, MD; Tamara Kaplan, MD; Discussant |
| 1:50 | Q&A |
| 1:55 | Approach to the Dizzy Patient | Manali Sheth, MD |
| 2:25 | Test Your Knowledge | Galina Gheihman, MD; Tamara Kaplan, MD; Discussant |
| 2:35 | Q&A |
| 2:40 | BREAK |
| 2:55 | Introduction to Neuropathies and Radiculopathies | Meabh O’Hare, MD |
| 3:35 | Test Your Knowledge | Galina Gheihman, MD; Tamara Kaplan, MD; Discussant |
| 3:45 | Q&A |
| 3:50 | End of Day Wrap-Up and Final Q&A |
| 4:00pm | Adjourn |
Optional Asynchronous Session (video posted to website)
- Introduction to Myasthenia Gravis and Muscle Diseases (40 minutes) | Joome Suh, MD
Tuesday, June 10, 2025 | 9:00am - 4:00pm | Virtual
Common Emergency Department and Inpatient Presentations
| 9:00am | Welcome & Introduction | Galina Gheihman, MD and Tamara Kaplan, MD |
| 9:05 | Recognizing and Managing Acute Stroke | Simona Nedelcu, MD, PhD |
| 9:40 | Test Your Knowledge | Galina Gheihman, MD; Tamara Kaplan, MD; Discussant |
| 9:50 | Q&A |
| 9:55 | Secondary Stroke Prevention | Alexis Roy, MD |
| 10:35 | Test Your Knowledge | Galina Gheihman, MD; Tamara Kaplan, MD; Discussant |
| 10:45 | Q&A |
| 10:50 | BREAK |
| 11:05 | Seizure Mimicks | Jong Woo Lee, MD, PhD |
| 11:40 | Test Your Knowledge | Galina Gheihman, MD; Tamara Kaplan, MD; Discussant |
| 11:50 | Q&A |
| 11:55 | Lunch |
| 1:00pm | Vision Loss: Differential Diagnosis | Sarah B. Conway, MD |
| 1:35 | Test Your Knowledge | Galina Gheihman, MD; Tamara Kaplan, MD; Discussant |
| 1:45 | Q&A |
| 1:50 | Living With MS: Supporting Quality of Life | Tamara Kaplan, MD |
| 2:20 | Test Your Knowledge | Galina Gheihman, MD; Tamara Kaplan, MD; Discussant |
| 2:30 | Q&A |
| 2:35 | BREAK |
| 2:50 | Back and Neck Pain | Shamik Bhattacharyya, MD |
| 3:30 | Test Your Knowledge | Galina Gheihman, MD; Tamara Kaplan, MD; Discussant |
| 3:40 | Q&A |
| 3:45 | End of Day Wrap-Up and Final Q&A |
| 4:00pm | Adjourn |
Optional Asynchronous Sessions (videos posted to website)
- Acute Stroke Management (40 minutes) | Sam Snider, MD
- Basics of Seizure Management (30 minutes) | Jong Woo Lee, MD, PhD
- What’s New in MS? (15 minutes) | Sarah B. Conway, MD
- Can’t Miss Neurological Infections (35 minutes) | George K. Harrold, MD
Wednesday, June 11, 2025 | 9:00am - 4:15pm | Virtual
Neurodegenerative Conditions & Other Chronic Presentations
| 9:00am | Welcome & Introduction | Galina Gheihman, MD and Tamara Kaplan, MD |
| 9:05 | Parkinson’s Disease and other Movement Disorders | Emily A. Ferenczi, MD, PhD |
| 9:45 | Test Your Knowledge | Galina Gheihman, MD; Tamara Kaplan, MD; Discussant |
| 9:55 | Q&A |
| 10:00 | Functional Neurologic Disorders | Angela O'Neal, MD |
| 10:35 | Test Your Knowledge | Galina Gheihman, MD; Tamara Kaplan, MD; Discussant |
| 10:45 | Q&A |
| 10:50 | BREAK |
| 11:05 | Evaluating Cognitive Disorders and Dementia | Seth Gale, MD |
| 11:45 | Test Your Knowledge | Galina Gheihman, MD; Tamara Kaplan, MD; Discussant |
| 11:55 | Q&A |
| 12:00pm | Lunch |
| 1:00 | Treatment & Management of Alzheimer’s Disease | Sheena Baratono, MD, PhD |
| 1:30 | Test Your Knowledge | Galina Gheihman, MD; Tamara Kaplan, MD; Discussant |
| 1:40 | Q&A |
| 1:45 | Sports Neurology | Claus Reinsberger, MD |
| 2:25 | Q&A |
| 2:35 | BREAK |
| 2:45 | Common Neurologic Complications of Cancer & Their Management | Eudocia Q. Lee, MD, MPH |
| 3:25 | Q&A |
| 3:30 | Three Mystery Cases: Test Your Knowledge! | Galina Gheihman, MD; Tamara Kaplan, MD |
| 4:00 | End of Day Wrap-Up and Final Q&A |
| 4:15pm | Adjourn |
Optional Asynchronous Sessions (videos posted to website)
- Complications of New Alzheimer’s Disease Treatments (30 minutes) | Sheena Baratono, MD, PhD
- What You Need to Know about Women’s Neurology (35 minutes) | Kenda Alhadid, MD
- Below the Belt Neurology (30 minutes) | Tamara B. Kaplan, MD
Thursday, June 12, 2025 | 9:00am - 12:30pm | In-Person (Somerville, MA)
Additional In-Person Workshop: Mastering the Neurological Examination
Join us for an interactive, in-person, hands-on workshop prepared by expert neurology faculty and APPs. This workshop is specifically tailored to teach non-neurology clinicians, including hospital-based and outpatient MDs and APPs basic and advanced neurological examination skills. We will focus on the assessment of common neurological concerns including weakness, dizziness, altered mental status, and gait abnormalities, and review an approach to the exam tailored for each presentation. We will review performing the neurological exam including special maneovers. There will be plenty of time for hands-on practice, with real-time feedback and coaching from our expert instructors.
| 9:00am | Welcome & Introduction; Overview of 4 Stations and Objectives for the Day | Galina Gheihman, MD and Tamara Kaplan, MD |
| 9:15 | Rotation 1: Approach to Weakness | Tamara Kaplan, MD; Margaret Naclerio, PA-C; Denis Balaban, MD; Ariel Nowicki, PA-C; Galina Gheihman, MD |
| 9:55 | BREAK |
| 10:00 | Rotation 2: Approach to Dizziness | Tamara Kaplan, MD; Margaret Naclerio, PA-C; Denis Balaban, MD; Ariel Nowicki, PA-C; Galina Gheihman, MD |
| 10:40 | BREAK |
| 10:45 | Rotation 3: Approach to Altered Mental Status | Tamara Kaplan, MD; Margaret Naclerio, PA-C; Denis Balaban, MD; Ariel Nowicki, PA-C; Galina Gheihman, MD |
| 11:25 | BREAK |
| 11:30 | Rotation 4: Approach to Gait Testing | Tamara Kaplan, MD; Margaret Naclerio, PA-C; Denis Balaban, MD; Ariel Nowicki, PA-C; Galina Gheihman, MD |
| 12:10pm | BREAK |
| 12:15 | Course Wrap-Up and Final Q&A | Tamara Kaplan, MD; Margaret Naclerio, PA-C; Denis Balaban, MD; Ariel Nowicki, PA-C; Galina Gheihman, MD |
| 12:30pm | Adjourn |
MGB EMPLOYEES
40% Discount available for MGB employees, please enter your discount code to receive this at registration. If you do not have a discount code but are interested in the course, please reach out to jrodriquez@bwh.harvard.edu from your MGB email to request it.
Virtual Course + In-Person Workshop
| Tuition Type | Tuition Fee |
Physician (MD/DO) | $1000 |
Nurse (RN/APRN), Physician Assistant, Allied Health Professional/Other | $700 |
Medical Student, Resident, or Fellow (Trainee) | $300 |
Virtual Course ONLY
| Tuition Type | Early Bird Tuition Fee (ends April 7) | Regular Tuition (After April 7) |
Physician (MD/DO) | $600 | $650 |
Nurse (RN/APRN), Physician Assistant, Allied Health Professional/Other | $400 | $450 |
Medical Student, Resident, or Fellow (Trainee) | $150 | $200 |
In-Person Workshop ONLY
| Tuition Type | Tuition Fee |
Physician (MD/DO) | $500 |
Nurse (RN/APRN), Physician Assistant, Allied Health Professional/Other | $400 |
Medical Student, Resident, or Fellow (Trainee) | $150 |
Cancellation Policy:
Registrations cancelled on or before May 26, 2025 will be refunded, less a $65 administrative fee. Registrations cancelled after May 26, 2025 will not be refunded.
Contact mgbcpd@mgb.org if you require assistance in cancelling your online registration.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for Specialty Physicians, Primary Care Physicians, APPs (PA and NP), General Practice Providers (primary care, family medicine), Internal Medicine, Emergency Medicine, Oncology, Geriatrics, Psychiatry, and Neurosurgery.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3684 [id] => 3684 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Brigham and Women's Hospital, Department of Neurology and Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=52304
[first] => https://cpd.partners.org/node?nid=52304&page=0
[last] => https://cpd.partners.org/node?nid=52304&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Mass General Brigham designates this enduring material for a maximum of 4.00 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Disclosure Summary of Relevant Financial Relationships
INELIGIBLE COMPANIES
Companies that are ineligible to be accredited in the ACCME System (ineligible companies) are those whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients. Examples of such organizations include:
- Advertising, marketing, or communication firms whose clients are ineligible companies
- Bio-medical startups that have begun a governmental regulatory approval process
- Compounding pharmacies that manufacture proprietary compounds
- Device manufacturers or distributors
- Diagnostic labs that sell proprietary products
- Growers, distributors, manufacturers or sellers of medical foods and dietary supplements
- Manufacturers of health-related wearable products
- Pharmaceutical companies or distributors
- Pharmacy benefit managers
- Reagent manufacturers or sellers
For more information: https://accme.org/faq/what-accmes-definition-ineligible-company
MITIGATION STRATEGIES
Mass General Brigham has implemented a process to mitigate relevant financial relationships for this continuing education (CE) activity to help ensure content objectivity, independence, fair balance and ensure that the content is aligned with the interest of the public.
The following planners have reported no relevant financial relationship with an ineligible company:
Lauren Hall, MD
Christa Nnoromele, MD
Chloe Slocum, MD, MPH
The following faculty have reported no relevant financial relationship with an ineligible company:
Marie Clark
Lauren Hall, MD
Christa Nnoromele, MD
Chloe Slocum, MD, MPH
Ryan VanVugt
Women with spinal cord injury (SCI) face barriers to health care that may lead to medical conditions going unrecognized or untreated due to attitudinal, environmental, economic, and informational barriers as they navigate the health care system. This educational course will help providers who serve women with SCI build capacity to provide optimal care for women with SCI by reviewing important aspects of primary and specialty care for women with SCI, including:
- Health maintenance, well-being, and accessibility
- General medical issues related to SCI
- Sexual and reproductive health
- Pregnancy and peripartum care
Target Audience
This activity is intended for physicians from multiple disciplines.
Learning Objectives
Upon completion of this activity, participants will be able to:
- Review elements of effective interprofessional care teams providing comprehensive carefor women with SCI.
- Identify relevant components of prenatal care women with SCI.
- Describe the importance of facility accessibility for providing care for women with SCI.
- Formulate a plan for appropriate health maintenance measures and preventive healthscreening for a woman with SCI based on her age and personal and family history.
Format
This course uses an innovative adaptive learning platform that presents content customized to each learner depending on their baseline level of expertise.
[summary] => [format] => full_html ) [field_course_transcript] => 1 [field_enrollment_requirement_min] => [field_enrollment_requirements] => Array ( ) [field_faculty_credentials] => Array ( [value] =>Course Director
Chloe Slocum, MD, MPH
Associate Director of Quality, Spaulding Rehabilitation Network, Mass General Brigham
Assistant Professor of Physical Medicine and Rehabilitation, Harvard Medical School
Director of Health Policy, Harvard Medical School Department of Physical Medicine and Rehabilitation
This course uses an innovative adaptive learning platform that presents content customized to each learner depending on their baseline level of expertise.
[format] => full_html ) [field_registration_instructions] => Array ( [value] =>INSTRUCTIONS
This activity consists of 4 modules. This course uses an innovative adaptive learning platform that presents content customized to each learner depending on their baseline level of expertise.
You may complete the modules in any order. After you have completed each module, return to this page to access the next module.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/2316 [id] => 2316 [resource] => accme_data ) [field_show_on_calendar] => [field_custom_provided] => Array ( [value] =>Spaulding Rehabilitation Network, Craig H. Neilsen Foundation & Mass General Brigham
[summary] => [format] => full_html ) [field_course_exhibitor] => Array ( ) [field_course_qualifiers] => Array ( ) [field_course_image_cards] => Array ( ) [field_income_expense] => Array ( ) [og_membership] => Array ( ) [og_membership__1] => Array ( ) [og_membership__2] => Array ( ) [og_membership__3] => Array ( ) [og_group_ref__og_membership] => Array ( ) [og_group_ref__og_membership__1] => Array ( ) [og_group_ref__og_membership__2] => Array ( ) [og_group_ref__og_membership__3] => Array ( ) [flag_course_bookmark_user] => Array ( [0] => Array ( [uri] => https://cpd.partners.org/user/156073 [id] => 156073 [resource] => user [uuid] => fab42c4b-4f26-4880-b8d3-ff46a5f41ce8 ) [1] => Array ( [uri] => https://cpd.partners.org/user/155194 [id] => 155194 [resource] => user [uuid] => d4bedef1-46c6-4f73-997f-41e4640849ae ) [2] => Array ( [uri] => https://cpd.partners.org/user/51046 [id] => 51046 [resource] => user [uuid] => 5f6c61f3-62bd-4120-872a-6b89c88f5198 ) [3] => Array ( [uri] => https://cpd.partners.org/user/141063 [id] => 141063 [resource] => user [uuid] => 13b1ecc4-52b0-469d-8dd9-15b40f0ab44e ) [4] => Array ( [uri] => https://cpd.partners.org/user/139811 [id] => 139811 [resource] => user [uuid] => 66263802-86d0-4813-ac8a-65e345a79b8a ) [5] => Array ( [uri] => https://cpd.partners.org/user/134808 [id] => 134808 [resource] => user [uuid] => e7f7966c-f5c5-4c13-ae10-ac20c42a046d ) [6] => Array ( [uri] => https://cpd.partners.org/user/75837 [id] => 75837 [resource] => user [uuid] => be7d19f0-1958-4de0-9cfd-fd6c28f3f100 ) [7] => Array ( [uri] => https://cpd.partners.org/user/101186 [id] => 101186 [resource] => user [uuid] => cb22822e-484c-4515-88ea-0520224b7148 ) [8] => Array ( [uri] => https://cpd.partners.org/user/14701 [id] => 14701 [resource] => user [uuid] => 20b260e8-68fa-49a1-ba78-81dec6a06724 ) [9] => Array ( [uri] => https://cpd.partners.org/user/90912 [id] => 90912 [resource] => user [uuid] => ef2585d9-66a1-4e25-aef0-cf8abfe72184 ) ) [model] => course_52304 [list_price] => 0.00000 [cost] => 0.00000 [sell_price] => 0.00000 [price] => 0.00000 [weight] => 0 [weight_units] => lb [length] => 0 [width] => 0 [height] => 0 [length_units] => in [pkg_qty] => 1 [ordering] => 0 [shippable] => 0 [nid] => 52304 [vid] => 225822 [is_new] => [type] => course [title] => Building Provider Capacity for Women with Spinal Cord Injury (SCI) [language] => und [url] => https://cpd.partners.org/content/building-provider-capacity-women-spinal-cord-injury-sci [edit_url] => https://cpd.partners.org/node/52304/edit [status] => 1 [promote] => 0 [sticky] => 0 [created] => 1662567633 [changed] => 1742572874 [author] => Array ( [uri] => https://cpd.partners.org/user/316 [id] => 316 [resource] => user [uuid] => d6db325c-6680-48ed-a601-f114e3fb592a ) [log] => [revision] => [course] => Array ( [uri] => https://cpd.partners.org/course/52304 [id] => 52304 [resource] => course ) [book_ancestors] => Array ( ) [comment] => 1 [comments] => Array ( ) [comment_count] => 0 [comment_count_new] => 0 [body] => Array ( ) [feeds_item_guid] => [feeds_item_url] => [feed_nid] => [relation_faculty_user] => Array ( ) [uuid] => e7569f12-f571-4aa7-8398-3b91f76df71d [vuuid] => c87a73f0-8a09-40aa-a60f-cf1367685223 ) ) )Array
(
[self] => https://cpd.partners.org/node?nid=70662
[first] => https://cpd.partners.org/node?nid=70662&page=0
[last] => https://cpd.partners.org/node?nid=70662&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
Nursing
Mass General Brigham designates this activity for 5.90 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
Physician Assistants
Mass General Brigham has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 6.25 AAPA Category 1 CME credits. Approval is valid until June 2025. PAs should only claim credit commensurate with the extent of their participation.

[summary] =>
[format] => full_html
)
[field_course_catalog] =>
[field_course_category] => Array
(
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1719237600
[value2] => 1782359940
[duration] => 63122340
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/71672
[id] => 71672
[resource] => file
[uuid] => 686a5cde-45b6-4c09-bdca-f6603f003f47
)
)
[field_course_intro] => Array
(
)
[field_course_live] =>
[field_course_location] => Array
(
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => Becoming an Asthma Educator is an on-line program with current information on asthma diagnosis, assessment, and treatment. It consists of a series of 9 video recordings, each approximately 40-45 minutes in length, and each followed by self-assessment multiple -choice questions with discussion of correct answers. It is designed to help allied health professionals to become qualified asthma educators.
- Module #1 Understanding & Teaching the Mechanisms of Asthma
- Module #2 Diagnosis & Assessment of Asthma
- Module #3 Introduction to Pulmonary Function Testing
- Module #4 Ambulatory Management of Asthma in the Adult
- Module #5 Special Considerations in Children
- Module #6 Assessing & Managing Allergic Sensitivities
- Module #7 Inhalers & Other Asthma-Related Devices
- Module #8 Managing Exacerbations of Asthma
- Module #9 Developing an Asthma Action Plan
learn more about this course from Dr. Chris Fanta:
- Initial Launch: June 2024
- This course is due to be renewed & reaccredited in June 2025
Christopher H. Fanta, MD - Course Co-Director
Mass General Brigham Asthma Center, Pulmonary & Critical Care Medicine
Brigham & Women's Hospital
Kenan Haver, MD - Course Co-Director
Pulmonary Medicine, Boston Children's Hospital
Elizabeth Klements, MS, RN, PPCNP-BC, AE-C
Boston Children's Hospital (retired)
Disclosure Summary of Relevant Financial Relationships
MITIGATION STRATEGIES
Mass General Brigham has implemented a process to mitigate relevant financial relationships for this continuing education (CE) activity to help ensure content objectivity, independence, fair balance and ensure that the content is aligned with the interest of the public.
The following planners have no reported relevant financial relationships with an ineligible company:
Christopher H. Fanta, MD
Victoria Forth, PA-C
Elizabeth Klements, MS, RN, PPCNP-BC, AE-C
The following speakers have reported no relevant financial relationships with an ineligible company:
Christopher H. Fanta, MD
Kenan Haver, MD
Elizabeth Klements, MS, RN, PPCNP-BC, AE-C
Upon completion of this activity, participants will be able to:
- Describe to patients and their families about asthma; allergy testing; proper medication use; and peak flow monitoring.
- Demonstrate a basic understanding of the use of pulmonary function testing in the diagnosis and assessment of asthma.
- Specify the distinction between asthma severity and asthma control, and employ techniques to help patients develop a strategy to achieve good asthma control.
- Acquire and demonstrate a willingness to collaborate across disciplines in asthma education. Both nurses and respiratory therapists are asked to administer inhaled medications to patients with asthma and teach skills (like peak flow monitoring) useful in preventing asthma attacks. Attendees are encouraged to recognize the unique set of skills brought to bear by each discipline.
- For technical support or questions regarding CEs, please contact Maxine Harney at the MGB Office of Continuing Professional Development.
- For medical questions about asthma, please contact Christopher Fanta, MD
This activity is intended for nurses, physician assistants, pharmacists, and other advanced practitioners.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3193 [id] => 3193 [resource] => accme_data ) [field_show_on_calendar] => [field_custom_provided] => Array ( [value] =>Mass General Brigham Asthma Center & Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=57480
[first] => https://cpd.partners.org/node?nid=57480&page=0
[last] => https://cpd.partners.org/node?nid=57480&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, this activity has been planned and implemented by Mass General Brigham and Cabo Verdean American Medical Society. Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this live activity for a maximum of 7.00 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 7.00 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
Psychology
7.00 Continuing Education (CE) credits are awarded.
Social Work
As a Jointly Accredited Organization, Mass General Brigham is approved to offer social work continuing education by the Association of Social Work Boards (ASWB) Approved Continuing Education (ACE) program. Organizations, not individual courses, are approved under this program. State and provincial regulatory boards have the final authority to determine whether an individual course may be accepted for continuing education credit. Mass General Brigham maintains responsibility for this course. Social workers completing this course receive 7.00 continuing education credit.
Lifelong Learning Maintenance of Certification (MOC) Program
MOC RECOGNITION STATEMENT
Successful completion of this CME activity, which includes participation in the evaluation component, enables the learner to earn credit toward the CME requirement of the American Board of Surgery’s Continuous Certification program. It is the CME activity provider's responsibility to submit learner completion information to ACCME for the purpose of granting ABS credit.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1685556000
[value2] => 1700456340
[duration] => 14900340
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1696593600
[value2] => 1696694400
[duration] => 100800
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/52351
[id] => 52351
[resource] => file
[uuid] => b49dd10c-52b1-46a8-a237-5178ce157988
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 44448
[latitude] => 0.000000
[longitude] => 0.000000
[name] => O'Keefe Auditorium - Massachusetts General Hospital
[street] => 55 Fruit Street
[additional] =>
[city] => Boston
[province] => MA
[postal_code] => 02114
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => Participants will gain an understanding of the healthcare delivery system and the social and economic factors affecting the health of Cabo Verdeans. Through interactive presentations and discussions by CVAMS members, the audience will learn about various topics in surgery, cardiology, preventative care, oncology, palliative care, mental health and education. In a concurrent mental health symposium participants will gain an understanding of trauma informed care. Attendees will be able to formulate goals to help improve health outcomes in Cabo Verde and the diaspora.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Course Co-Directors
Doreen Defaria Yeh, MD
Associate Director, MGH Adult Congenital Heart Disease Program
Co-Director, MGH Cardiovascular Disease and Pregnancy Program
Program Director, Cardiovascular Disease Fellowship, Massachusetts General Hospital
Madelaine Tully, MD
Family Physician, Progressive Community Health Center
Milwaukee, Wisconsin
Planning Committee
Julio Teixeira, MD, FACS
President of CVAMS
Director of Minimally Invasive Surgery, Northwell Health
New York
Patricia Andrade, MD
Physician, General Surgeon
Taunton and Fall River, MA
Elizabeth Gomes, DO
Physician, Jenks Park Pediatrics Women and Infant's Hospital through Care - New England
Central Falls, RI | Providence, RI
Maria Fatima Barros, RN, MSN
(Retired) Volunteer many communities’ health & advisory committees, RI Department of Health Advisory Boards
Providence, RI
Rosilda James, PsyD
Clinical Psychologist, Alves Psychotherapy
Walnut Creek, CA
Samora Miguel Cardoso Lopes
Clinical Research Sub-investigator, Department of Anesthesia, Critical Care And Pain Medicine
Harvard Medical Faculty Physicians
Beth Israel Deaconess Medical Center
Boston, MA
Maya Spencer, MD
Pediatrician, Atrius Health
Braintree, MA
Susan Weinberg, MD, FACR
Founder, Mary Jo Cropper Family Center for Breast Care
Past Director of Trihealth Radiology, Cincinnati
Rad Partners—SEAL Team
Lyla Blake, MD, MPH
Physician, Community Health Center of Cape Cod
Falmouth, MA
Kimberly Coto, LICSW, MSW
Clinical Social Work/Therapist
New Bedford, MA
Faculty
Patrice Alves, MD
Internal Medicine Physician, Christus Health
San Antonio, TX
Paulo Pina, MD
Network Pediatric Medical Director, Family Health Centers at NYU Langone
Brooklyn, NY
Maritsa Barros, EdD, MS
University Lecturer, Tufts University
Owner, Senavision
Carla Barbosa, MD
National Program Coordinator for Oncology
Ministry of Health, Cabo Verde
Hirondina Borges, MD
Oncologist, Agostinho Neto University Hospital
Praia, Cabo Verde
Adriano Cabral, MEd, CAGS
CEO, Inclusion Family Center, Inc.
Brockton, MA
Samantha DeAndrade, MD, MPH
Fellow in Urogynecology, Harbor-UCLA Medical Center
Los Angeles, CA
Luis Manuel Dias Andrade, MD
Physician, Agostinho Neto University Hospital
Praia, Cabo Verde
David Earle, MD, FACS
Director, New England Hernia Center
Associate Professor of Surgery, Tufts University – School of Medicine
Medical Advisor, Western Mass Region of the National Ski Patrol
Oyere K. Onuma, MD
Director, Global Cardiovascular Health Program at Massachusetts General Hospital – Cardiology Division & Corrigan Minehan Heart Center
Assistant Professor of Medicine, Harvard Medical School
Associate Director, Health Equity in Cardiology (MGH)
E. Isabel Lopes, MD
Physician, Mad River Community Hospital, Open Door Community Health Center & Providence Redwood Memorial Hospital
California, USA
Antonio Mendes, MD
Medical Director, Mendes Medical Associates
Norwood, MA
Robert M. Teixeira, MD
Assistant Professor of Surgery, University of Utah
Salt Lake City, UT
Danielson Pereira Barreto da Veiga, MD
President, Order of Physicians, Cabo Verde
Chair of Surgery, Agostinho Neto University Hospital
Nicholas Tawa, MD
Assistant Professor of Surgery, Harvard Medical School
Associate Director of Nutrition Support Service, Beth Israel Deaconess Medical Center
Nivia Vieira, MSc
Assistant Director of Healthcare Partnership, Project Bread
East Boston, MA
Idalina S. Afopa, FNP-BC
Family Nurse Practitioner, Veterans Health Administration
Medical Center, Manhattan, New York, NY
Valéria Semedo, MD
Physician, Agostinho Neto University Hospital
Coordinator, HAN – Palliative Care
Member, African Association of Palliative Care
Lecturer, University of Cape Verde
Nursing Chair, Disability Verification Commission of the National Social Security Institute
Cabo Verde
Jason Sherer, MD, MPH
Physician, Cardiology - St. Francis Heart Center
Rockville Centre, NY
Darlene Spencer
Program Officer/Board President, Carney Family Charitable Foundation
Cape Verdean Association in New Bedford
Joseph Gomes, DO
Emergency Medicine Physician, Memorial Hospital West
Pembroke, FL
Merrian Brooks, MD
Attending Pediatrician/Adolescent Medicine Specialist, Craig Dalsimer Division of Adolescent Medicine, Children's Hospital of Philadelphia
Philadelphia, PA
Anibal Melo, MD
Physician, Saint Luke’s Hospital – Department of Nephrology
St. Louis, MO
Djanira Fernandes, MD
PGY1 Resident, Beth Israel Deaconess Medical Center
Tim Johnson, MD
Orthopedic Surgeon, Johns Hopkins School of Medicine
Assistant Professor of Sports Medicine, Shoulder & Elbow Surgery, Johns Hopkins School of Medicine
Elisa Cabral, MS
Inclusion Family Center
Claudia Fontes, MD
Pediatric Emergency Medicine
Fresno, CA
Roberto Pineda, MD
Thomas Y. & Clara W. Butler Chair of Ophthalmology, Massachusetts Eye & Ear
Associate Professor of Ophthalmology, Harvard Medical School
Gabriella Spinola
Chief Marketing Officer, CMO
WeCare 365 AFC
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Recognize the unique causes of morbidity and mortality in Cabo Verde and the diaspora.
- List specific challenges identified by the CVAMS teams in the areas of cardiology, preventive medicine, surgery, and mental health.
- Use the experiences and data from the recent scientific exchange to identify opportunities for future collaborations and enhance public health priorities and building sustainable infrastructure.
- Acquire tools to practice trauma informed care in a clinical setting. Realize the importance of client-provider relationship building to support healing.
- Identify the signs of burn-out and accumulative stress in one’s self and others. Create a self-care plan through an interactive workshop.
- Identify implicit bias and build awareness as they relate to delivering trauma informed care.
- Recognize the significance of colonial trauma, immigration, assimilation, colorism, family separation and classism.
[format] => full_html
)
[field_program] => Array
(
[value] =>
[format] => full_html
)
[field_registration_instructions] => Array
(
[value] => | Registration Type | Tuition Fee |
|---|---|
| All Health Practitioners | $75 |
| General Public | Free |
| Residents, Fellows & Students | Free |
Cancellation Policy:
Registrations cancelled on or before September 22, 2023 will be refunded, less a $15 administrative fee. Registrations cancelled after September 22, 2023 will not be refunded.
Contact partnerscpd@partners.org if you require assistance in cancelling your online registration.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for physicians, nurses, nurse practitioners, psychologists, physician assistants, social workers, other members of the healthcare team, and community members.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/2717 [id] => 2717 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>The Cabo Verdean American Medical Society & Mass General Brigham

[summary] => [format] => full_html ) [field_course_exhibitor] => Array ( ) [field_course_qualifiers] => Array ( ) [field_course_image_cards] => Array ( ) [field_income_expense] => Array ( ) [og_membership] => Array ( ) [og_membership__1] => Array ( ) [og_membership__2] => Array ( ) [og_membership__3] => Array ( ) [og_group_ref__og_membership] => Array ( ) [og_group_ref__og_membership__1] => Array ( ) [og_group_ref__og_membership__2] => Array ( ) [og_group_ref__og_membership__3] => Array ( ) [flag_course_bookmark_user] => Array ( [0] => Array ( [uri] => https://cpd.partners.org/user/122797 [id] => 122797 [resource] => user [uuid] => fd3c40ae-6449-4f84-86fb-5276cbe4cf87 ) [1] => Array ( [uri] => https://cpd.partners.org/user/122793 [id] => 122793 [resource] => user [uuid] => e28732ca-f88e-4ba2-9c6a-4b068199f8dc ) ) [model] => course_57480 [list_price] => 0.00000 [cost] => 0.00000 [sell_price] => 75.00000 [price] => 75.00000 [weight] => 0 [weight_units] => lb [length] => 0 [width] => 0 [height] => 0 [length_units] => in [pkg_qty] => 1 [ordering] => 0 [shippable] => 0 [nid] => 57480 [vid] => 177264 [is_new] => [type] => course [title] => Cabo Verdean American Medical Society: Bringing Morabeza to Medicine 2023 [language] => und [url] => https://cpd.partners.org/content/cabo-verdean-american-medical-society-bringing-morabeza-medicine-2023 [edit_url] => https://cpd.partners.org/node/57480/edit [status] => 1 [promote] => 0 [sticky] => 0 [created] => 1685558357 [changed] => 1700155650 [author] => Array ( [uri] => https://cpd.partners.org/user/316 [id] => 316 [resource] => user [uuid] => d6db325c-6680-48ed-a601-f114e3fb592a ) [log] => [revision] => [course] => Array ( [uri] => https://cpd.partners.org/course/57480 [id] => 57480 [resource] => course ) [book_ancestors] => Array ( ) [comment] => 1 [comments] => Array ( ) [comment_count] => 0 [comment_count_new] => 0 [body] => Array ( ) [feeds_item_guid] => [feeds_item_url] => [feed_nid] => [relation_faculty_user] => Array ( ) [uuid] => 000c2b56-6ea6-4909-9220-f83255f23cdd [vuuid] => 4da68cf5-b3c3-44ad-bfc6-a56115e8236e ) ) )
Array
(
[self] => https://cpd.partners.org/node?nid=65080
[first] => https://cpd.partners.org/node?nid=65080&page=0
[last] => https://cpd.partners.org/node?nid=65080&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => Accreditation
In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditTM
Mass General Brigham designates this live activity for a maximum of 1 AMA PRA Category 1 CreditTM. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 1 ANCC contact hour. Nurses should only claim credit commensurate with the extent of their participation in the activity.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1693929600
[value2] => 1717088400
[duration] => 23158800
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/238
[id] => 238
[resource] => taxonomy_term
[uuid] => fd81c17a-d19b-46b8-ad6b-2c5aee9ce9be
)
[1] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/237
[id] => 237
[resource] => taxonomy_term
[uuid] => 842d3b08-d27d-4a11-8281-71bcfb00ec51
)
[2] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/239
[id] => 239
[resource] => taxonomy_term
[uuid] => 8fe8f562-9596-41a9-8e2f-c93aa2c8dae9
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/54406
[id] => 54406
[resource] => file
[uuid] => 71939cdf-376f-4fbf-9bc0-e93579d78d2b
)
)
[field_course_intro] => Array
(
)
[field_course_live] =>
[field_course_location] => Array
(
[lid] => 45473
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Massachusetts General Hospital
[street] =>
[additional] =>
[city] => Boston
[province] => MA
[postal_code] => 02114
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => Massachusetts General Hospital
Cancer Center Grand Rounds 2023-2024
September 7, 2023 - May 30, 2024
For the first time ever, the 2023-2024 Cancer Center Grand Rounds are available to the public to attend virtually LIVE via paid subscription.
(Please note: This subscription does not include in-person attendance)
The theme of the series is "Women in Cancer: and kicks off Thursday September 7, 2023 at 12:00 PM EDT. with the annual "Chabner Pioneers in Oncology Lectureship". The series will cover a comprehensive array of disease areas and topics, attendees will be provided with a robust selection of sessions to bring them up to speed on the most cutting-edge research and therapies in oncology.
The subscription will provide access to BOTH the live webinar AND the recording; however, if claiming credit, you may only claim credit for attending one or the other per date.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Colin D. Weekes, MD, PhD - Course Director
Director, Medical Oncology Research for Pancreatic Cancer,
Director, Cancer Center Grand Rounds Program
Massachusetts General Hospital
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
[value] => Participation is online streaming – broadcast from Massachusetts General Hospital.
After you register, you will receive an email with details for how to participate.
[format] => full_html
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Evaluate recent advances or controversies in hematology/oncology treatment, clinical research and/or basic science investigation presented in this series
- Assess opportunities to integrate information, tools or practices presented in this conference into how you deliver or support research and patient care
- Apply new information or perspectives from this conference into specific aspects of your responsibilities in patient care, research or the system in which you work.
- Recognize evolving landscape of cancer care worldwide
[format] => full_html
)
[field_program] => Array
(
[value] => Sessions will be held weekly on Thursday from September 7, 2021 to May 30, 2022 from 12:00 to 1:00 PM.
September 7, 2023
The Chabner Pioneers in Oncology Lectureship – Precision Medicine for Primary and Metastatic Brain Tumors: From Bench to Bedside (and Back to Bench)
Priscilla Brastianos, MD
Mass General Cancer Center
September 28, 2023
(This session will be available to view LIVE ONLY. There will be no recording for this session.)
Structure and Function of Mammalian SWI/SNF Chromatin Remodeling Complexes in Cancer
Cigall Kadoch, PhD
Dana-Farber Cancer Institute
October 5, 2023
Talk Title Novel Therapeutics in Gynecologic Cancers
Roisin O’Cearbhaill, MD
Memorial Sloan-Kettering Cancer Center
October 12, 2023
Women in Cancer: Navigating the Glass Ceiling
Lisa Butterfield, PhD
University of California San Francisco
Kornelia Polyak, MD, PhD
Dana-Farber Cancer Institute
Noopur Raje, MD
Mass General Cancer Center
November 9, 2023
Achieving Success as A Square Peg in the Round Hole of Academic Medicine
Jennifer Temel, MD
Mass General Cancer Center
November 30, 2023
Female Participant Engagement in Cancer Research: Sample Programs from the Field to a Pandemic
Lourdes Baezconde-Garbanati, PhD
University of Southern California
December 7, 2023
The Dobbs Decision: Implications for Women’s Health and Cancer Care
Lisa Barroilhet, MD
University of Wisconsin School of Medicine and Public Health
December 14, 2023
Targeted Therapy for Premenopausal Early Breast Cancer: A 100 Year Old Strategy
Sandra Swain, MD
Georgetown University Medical Center
Spring 2024 Grand Rounds Schedule
January 4, 2024
ASH Update
Classical Heme (Jonathan Carlson)
Leukemia (Rupa Narayan)
Lymphoma (Jake Soumerai)
Myeloma (Diana Cirstea)
BMT (Richard Newcomb)
Cell Therapy (Mark Leick)
January 11, 2024
Integrating Clinical and Laboratory Research to Identify Mechanisms of Response and Resistance to Immune Checkpoint Therapy
Padmanee Sharma, MD, PhD
MD Anderson Cancer Center
January 18, 2024
From the Ether Dome to Seldin Plaza: My Path in Renal Cell Carcinoma
Tian Zhang, MD
UT Southwestern Medical Center
January 25, 2024
Can’t Stop, Won’t Stop: The Development of New Therapies, and New Trialists, Toward a Future of Cure
Janice Mehnert, MD
NYU Langone Health
February 8, 2024
Advocacy in Oncology: Connecting What Matters with Our Science and Care
Pamela Kunz, MD
Yale School of Medicine
February 29, 2024
Brain Metastases of Breast Cancer
Patricia Steeg, PhD
National Institutes of Health
March 14, 2024
Rethinking Radiation Oncology Using HPV Driven Oropharyngeal Carcinoma as a Model
Nancy Lee, MD, FASTRO
Memorial Sloan Kettering Cancer Center
March 21, 2024
Bridging the GAP While Shattering Ceiling
Rachna Shroff, MD, MS, FASCO
University of Arizona Cancer Center
March 28, 2024
Porphyria: New Therapies and Research
Rebecca Karp, MD
Massachusetts General Hospital
Amy Dickey, MD, MSc
Massachusetts General Hospital
April 25, 2024
Treating AML in 2024 : Individualizing Treatment Approaches with Novel Therapies
Courtney DiNardo, MD, MSCE
MD Anderson Cancer Center
[format] => full_html
)
[field_registration_instructions] => Array
(
[value] => | Registration Type | Tuition Price |
|---|---|
| All Other Healthcare Providers | $250.00 |
| Fellows | $50.00 |
For questions regarding the registration process, please contact Mass General Brigham Office of Continuing Professional Development at partnerscpd@partners.org.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for research and clinical staff who need to be educated on cutting edge information on advances and perspectives on cancer research and treatment across the full spectrum of cancer specialization.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/2953 [id] => 2953 [resource] => accme_data ) [field_show_on_calendar] => [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital Cancer Center and Mass General Brigham
[summary] => [format] => full_html ) [field_course_exhibitor] => Array ( ) [field_course_qualifiers] => Array ( ) [field_course_image_cards] => Array ( ) [field_income_expense] => Array ( ) [og_membership] => Array ( ) [og_membership__1] => Array ( ) [og_membership__2] => Array ( ) [og_membership__3] => Array ( ) [og_group_ref__og_membership] => Array ( ) [og_group_ref__og_membership__1] => Array ( ) [og_group_ref__og_membership__2] => Array ( ) [og_group_ref__og_membership__3] => Array ( ) [flag_course_bookmark_user] => Array ( [0] => Array ( [uri] => https://cpd.partners.org/user/23537 [id] => 23537 [resource] => user [uuid] => 3c748a43-8ea3-40ff-94c8-7386da393143 ) [1] => Array ( [uri] => https://cpd.partners.org/user/18239 [id] => 18239 [resource] => user [uuid] => a141fe07-0879-4afe-b2b8-4ff1d8c0480b ) [2] => Array ( [uri] => https://cpd.partners.org/user/58483 [id] => 58483 [resource] => user [uuid] => 6f9fa7cd-2b4d-46ef-90df-21b9007cfcb4 ) [3] => Array ( [uri] => https://cpd.partners.org/user/120506 [id] => 120506 [resource] => user [uuid] => b05faaea-a162-4a41-831c-105748c49f8e ) ) [model] => course_65080 [list_price] => 0.00000 [cost] => 0.00000 [sell_price] => 250.00000 [price] => 250.00000 [weight] => 0 [weight_units] => lb [length] => 0 [width] => 0 [height] => 0 [length_units] => in [pkg_qty] => 1 [ordering] => 0 [shippable] => 0 [nid] => 65080 [vid] => 198190 [is_new] => [type] => course [title] => MGH Cancer Center Grand Rounds 2023-2024 - Subscription [language] => und [url] => https://cpd.partners.org/content/mgh-cancer-center-grand-rounds-2023-2024-subscription [edit_url] => https://cpd.partners.org/node/65080/edit [status] => 1 [promote] => 0 [sticky] => 0 [created] => 1693575060 [changed] => 1720704169 [author] => Array ( [uri] => https://cpd.partners.org/user/257 [id] => 257 [resource] => user [uuid] => bd6fd397-09cf-4275-a7d4-35783f50f323 ) [log] => [revision] => [course] => Array ( [uri] => https://cpd.partners.org/course/65080 [id] => 65080 [resource] => course ) [book_ancestors] => Array ( ) [comment] => 1 [comments] => Array ( ) [comment_count] => 0 [comment_count_new] => 0 [body] => Array ( ) [feeds_item_guid] => [feeds_item_url] => [feed_nid] => [relation_faculty_user] => Array ( ) [uuid] => 17788de8-02f6-48e7-891b-57f0471bd26f [vuuid] => d7e1c506-ae9c-4cad-aa41-4bae28e6dcb4 ) ) )Array
(
[self] => https://cpd.partners.org/node?nid=82032
[first] => https://cpd.partners.org/node?nid=82032&page=0
[last] => https://cpd.partners.org/node?nid=82032&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Mass General Brigham designates this live activity for a maximum of 7.75 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/235
[id] => 235
[resource] => taxonomy_term
[uuid] => d4487c25-fe2e-460a-b2b6-c180dcd804cc
)
[1] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/236
[id] => 236
[resource] => taxonomy_term
[uuid] => eb0ec44a-4c85-40f2-9c3b-b8a19a3d44a9
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1733413260
[value2] => 1749527940
[duration] => 16114680
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1746791100
[value2] => 1746824400
[duration] => 33300
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/239
[id] => 239
[resource] => taxonomy_term
[uuid] => 8fe8f562-9596-41a9-8e2f-c93aa2c8dae9
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/79028
[id] => 79028
[resource] => file
[uuid] => 8a77efc1-64bc-4462-a5c8-ed9cec900661
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => This is a virtual course
Midlife Women’s Health 2025 provides a multi-disciplinary approach to the care of menopausal women. Advances in research, technology, and pharmacology increase options available for midlife women, but this rapidly changing knowledge-base presents a challenge for clinicians. Care for women at this stage of life is optimized by education on a range of medical concerns provided by experts from a wide variety of medical specialties. Given demographic changes in the US population, midlife women are becoming an increasingly important group served by health care professionals, with needs that cross many areas of medical expertise.
In this educational activity, a multidisciplinary group of experts from Massachusetts General Hospital will present on the evaluation and management of osteoporosis, gastrointestinal malignancy, stress, obesity, substance use disorder, anxiety, sexual dysfunction, breast cancer, and menopausal hormone therapy to assist clinicians in caring for their midlife patients.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Jan Shifren, MD - Course Director Dr. Shifren is a reproductive endocrinologist at the Massachusetts General Hospital and Director of the MGH Midlife Women’s Health Center. She focuses her research on menopause, including the effects of estrogens, androgens and alternative therapies on menopausal symptoms and sexual function. She is a past President of the Menopause Society. |
Isaac Schiff, MD Dr. Isaac Schiff is the Chief, Department of Obstetrics and Gynecology, Emeritus, at the Massachusetts General Hospital and the Joe Vincent Meigs Distinguished Professor of Gynecology at Harvard Medical School. He is Co-Director of the MGH Midlife Women’s Health Center. Dr. Schiff is an internationally known expert in menopause, a founding member of the Menopause Society, and the Editor-in-Chief of the journal, Menopause. |
Daniel Chung, MD Dr. Daniel Chung is a gastroenterologist at the Massachusetts General Hospital and Director of the High-Risk GI Cancer Clinic. He is also Medical Co-Director of the Center for Cancer Risk Assessment. His research aims to gain new insights into the molecular pathogenesis of GI malignancies, with a focus on colon cancer, angiogenesis, hereditary cancers, and genetic instability. |
John Denninger, MD, PhD Dr. John Denninger is a psychiatrist at the Massachusetts General Hospital and Director of Integrative Science and Clinical Training at the Benson-Henry Institute for Mind Body Medicine. His research focuses on how mind-body interventions can promote wellness and resilience. He also investigates how these interventions work by exploring genes, biochemistry, and brain activity. |
Tara Iyer, MD Dr. Tara Iyer is a family medicine and obesity specialist and Medical Director of the Menopause and Midlife Clinic in the Division of Women's Health at the Brigham and Women’s Hospital. Her clinical and research interests include weight management in women, bone health, and menopause care of the cancer survivor. |
Linda Kelly, DNP, ANP-BC Dr. Linda Kelly is an advanced practice provider at the Massachusetts General Hospital. She is the Nursing Director of the Midlife Women's Health Center in the Department of Obstetrics and Gynecology at MGH. |
Noreen Reilly Harrington, PhD Dr. Noreen Harrington is a psychologist at the Massachusetts General Hospital. She is an internationally-recognized expert in the cognitive-behavioral treatment of mood and anxiety disorders, with a special focus on bipolar disorder. |
Kathryn Rexrode, MD, MPH Dr. Kathryn Rexrode is an internist and Chief of the Division of Women's Health in the Department of Medicine at the Brigham and Women’s Hospital. She leads efforts to advance women’s health through research, clinical care, medical education and advocacy. He work focuses on metabolic factors, hormonal exposures and sex-specific risk factors for cardiovascular disease. |
James Sawalla Guseh, II, MD Dr. Sawalla Guseh is a cardiologist at the Massachusetts General Hospital and Director of the Cardiovascular Performance Program. His principal clinical interests include the treatment of patients, professionals, and athletes with varied forms of heart disease. His research focuses on understanding the molecular basis of human aerobic fitness. |
Joy Tsai, MD Dr. Joy Tsai is an endocrinologist and osteoporosis specialist in the Division of Endocrinology in the Department of Medicine at the Massachusetts General Hospital. Her research interests include optimizing postmenopausal osteoporosis therapy and bone health, with a focus on the evaluation of bone quality through advanced imaging techniques. |
Francys Verdial, MD Dr. Francys Verdial is a surgical oncologist at the Massachusetts General Hospital with special expertise in the management of breast cancer. |
Sarah Wakeman, MD Dr. Sarah Wakeman is the Medical Director for the Massachusetts General Hospital Substance Use Disorder Initiative and the Senior Medical Director for Substance Use Disorder at Mass General Brigham. Her research interests include evaluating models for integrated substance use disorder treatment in general medical settings, recovery coaching, physician attitudes and practice related to substance use disorder, and screening for substance use in primary care. |
Upon completion of this activity, participants will be able to:
- Assess midlife women for osteoporosis and utilize effective therapies.
- Identify risk factors for gastrointestinal malignancies to optimize screening strategies and outcomes.
- Integrate mind body strategies to reduce the adverse impact of stress on midlife women's health.
- Recognize the link between exercise, obesity and cardiovascular disease in women to improve health.
- Assess midlife women for alcohol and opioid use disorder and guide the use of available treatment options.
- Employ a greater understanding of anxiety in women to reduce disease burden.
- Integrate behavioral and pharmacologic strategies to improve sexual function in women.
- Formulate a strategy to identify women at increased risk of breast cancer to optimize care.
- Evaluate symptomatic midlife women for menopausal hormone therapy, incorporating an individualized assessment of risks and benefits.
| 7:45am | Welcome & Introductory Remarks | Jan Shifren, MD |
| 8:00 | Osteoporosis: Treatment Options to Reduce Fracture Risk | Joy Tsai, MD |
| 8:35 | Q & A |
| 8:45 | Gastrointestinal Malignancy at Midlife: Risk Assessment & Screening Strategies | Daniel Chung, MD |
| 9:20 | Q & A |
| 9:30 | Stress Reduction at Midlife: A Mind Body Approach | John Denninger, MD, PhD |
| 10:05 | Q & A |
| 10:15 | Break |
| 10:30 | Battling the Bulge: Exercise, Weight & Cardiovascular Health at Midlife | James Sawalla Guseh, II, MD |
| 11:05 | Q & A |
| 11:15 | Alcohol & Opioid Use Disorder at Midlife: Optimizing Care | Sarah Wakeman, MD |
| 11:50 | Q & A |
| 12:00pm | Lunch Break |
| 1:00 | Anxiety in Midlife Women: Therapeutic Options | Noreen Reilly Harrington, PhD |
| 1:35 | Q & A |
| 1:45 | Sexual Dysfunction in Women: Causes & Care | Jan Shifren, MD |
| 2:20 | Q & A |
| 2:30 | Breast Cancer: Update on Screening Algorithms & Treatment Options | Francys Verdial, MD |
| 3:05 | Q & A |
| 3:15 | Break |
| 3:30 | Menopausal Hormone Therapy: Update for 2025 | Tara Iyer, MD |
| 4:05 | Q & A |
| 4:15 | Everything You Wanted to Know About Menopause, but Were Afraid to Ask | Isaac Schiff, MD; Katheryn Rexrode, MD, MPH & Linda Kelly, DNP, ANP-BC |
| 5:00pm | Adjourn |
[format] => full_html ) [field_registration_instructions] => Array ( [value] =>
BEFORE MARCH 28, 2025
| Registration Type | Tuition Fee |
|---|---|
| Physician | $270 |
| Other Health Care Professionals & Physicians-in-Training | $125 |
AFTER MARCH 28, 2025
| Registration Type | Tuition Fee |
|---|---|
| Physician | $295 |
| Other Health Care Professionals & Physicians-in-Training | $150 |
Cancellation Policy:
Registrations cancelled on or before March 28, 2025 will be refunded, less a $35 administrative fee. Registrations cancelled after March 28, 2025 will not be refunded.
Contact mgbcpd@mgb.org if you require assistance in cancelling your online registration.
Please contact our Course Coordinator at MGHMidlifeCenter@mgh.harvard.edu prior to the event to assist you with any special needs.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for physicians and advance practice nurses in primary care, gynecology, general surgery, internal medicine, endocrinology, psychiatry, gynecological oncology, cardiology, and preventive medicine who provide care to midlife women. Physicians and advance practice nurses in-training also are encouraged to attend.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3635 [id] => 3635 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital - Department of OB/GYN & Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=81608
[first] => https://cpd.partners.org/node?nid=81608&page=0
[last] => https://cpd.partners.org/node?nid=81608&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this live activity for a maximum of 20.25 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/540
[id] => 540
[resource] => taxonomy_term
[uuid] => e731fa5e-224d-48ef-a2bf-def1293fa566
)
[1] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/539
[id] => 539
[resource] => taxonomy_term
[uuid] => 57fa07dc-bb22-48eb-bff3-97c75764b9e6
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1730728800
[value2] => 1751687940
[duration] => 20959140
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1743681600
[value2] => 1743886800
[duration] => 205200
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/238
[id] => 238
[resource] => taxonomy_term
[uuid] => fd81c17a-d19b-46b8-ad6b-2c5aee9ce9be
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/77642
[id] => 77642
[resource] => file
[uuid] => 44fa0bec-301e-4e67-a94c-411d284e71db
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 56788
[latitude] => 0.000000
[longitude] => 0.000000
[name] => W Boston
[street] => 100 Stuart Street
[additional] =>
[city] => Boston
[province] => MA
[postal_code] => 02116
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => Please Note: The Anal Fistula/Pilonidal Cadaver Workshop is SOLD OUT

Harvard Medical School (HMS) faculty will be joined by renowned national and international experts from the International Society of University Colon and Rectal Surgeons (ISUCRS) to explore the latest advancements in surgical treatments for benign diseases of the colon and rectum. The program will feature hands-on cadaver courses, co-taught by Harvard faculty and distinguished leaders in the field, including Dr. Arun Rojanasakul (Thailand), Dr. Gabriela Möslein (Germany), Dr. Mark Soliman (USA), and Dr. Stephen Goldstone (USA), who have graciously agreed to serve as guest workshop co-directors. These sessions will provide unforgettable hands-on experiences, covering topics such as anal fistula, pilonidal disease, robotic surgery, laparoscopic techniques, and HRA procedures.
The event will also include two days of live and virtual lecture sessions, featuring updates from world-class surgeons from around the globe, including Dr. Joseph Nunoo Mensah (UK), Dr. Lucia Oliveira (Brazil), Dr. Carlo Ratto (Italy), Dr. Ayca Gultekin (Turkey), Dr. Gonsalo Hagerman (Mexico), and many others. Live and virtual lectures will be enhanced with videos and interactive content, offering participants a comprehensive learning experience. Expect spirited debates and challenging case discussions, ensuring a dynamic and engaging experience for both seasoned surgeons and novice colorectal learners.
Be sure to bring your APP team to learn alongside us while enjoying the charm of Boston in the spring, right in the heart of its historic downtown. Finally, for the brave at heart, join our poster competition! Three lucky winners will have the opportunity to present their work as part of our meeting and win cash prizes.
Special Discounts: ISUCRS members are eligible for a 15% discount, while surgeons from low-income countries can receive a 30% discount on registration fees.
Accommodations:
W Boston is offering a special group rate for attendees:
- $379.00 USD per night
- Room Type NOT Guaranteed
- Last Day to Book: Wednesday, March 19, 2025
Click here to book your group rate for MGH Colorectal Surgery Course
[summary] => [format] => full_html ) [field_course_transcript] => 1 [field_enrollment_requirement_min] => [field_enrollment_requirements] => Array ( ) [field_faculty_credentials] => Array ( [value] =>
Course Directors
Liliana Bordeianou, MD
Professor of Surgery, Harvard Medical School;
Co-Director, MGH Pelvic Floor Disorders Center,
Co-Chair, Mass General Brigham Colorectal Surgery Collaborative,
Massachusetts General Hospital
Christy Cauley, MD
Assistant Professor Harvard Medical School;
Colorectal Surgeon, Gastrointestinal Surgeon
Massachusetts General Hospital
International Faculty
Joseph Nunoo Mensah, MD, FASCRS
Colorectal Surgeon at Kings College Hospital and Cleveland Clinic London,UK; Head of the Department of Colorectal Surgery; Former President of the International Society of University Colon and Rectal Surgeons (ISUCRS) from 2022-24.
Arun Rojanasakul, MD, FASCRS
Emeritus Prof at the Banpakok International Hospital in Bangkok, Thailand: Honorary FASCRS (USA), PSCS (Phillipines), ACRSI (India) and SSCS (Singapore) Fellow; Past president of the Colorectal Surgery Committee of Thailand and the Coloproctology Association of Asia-Pacific; Inventor of the LIFT (Ligation Intersphincteric Fistula Tract) Procedure
Lucia Oliveira, MD
Director of the Anorectal Physiology department, Cepemed, Rio de Janeiro, Brazil; Board Member of ALAPP (Latin American Pelvic Floor Society)
Carlo Ratto, MD, FASCRS
Prof. Ratto is the Chief of the Unit of Proctology and Pelvic Floor Surgery at the Isola Tiberina Gemelli Hospital in Rome, Italy, and Hon FASCRS (USA)
Ayca Gultekin, MD
Professor of Surgery, Zonguldak Bulent Ecevit University School of Medicine, Turkey; Editor in Chief, Turkish Journal of Colorectal Disease; Assistant Secretary, UEMS (European Union of Medical Specialists) Section of Surgery-Coloproctology; Chair of Pelvic Floor Disorders Group, Turkish Society of Colon and Rectal Surgery
Gabriela Möslein, MD
Professor of Surgery and Dept. Head of the newly established Center for Hereditary Tumors at the Academic Hospital of the University of Düsseldorf Ev. BETHESDA in Duisburg, Germany;
Director of InSiGHT (International Society for Hereditary Gastrointestinal Tumors)
Former Secretary of ESCP (European Society for Coloproctology) from 2016 – 2020 and ESCP Program Director(2020-2024)
Gonzalo Hagerman, MD , FASCRS
Professor, Universidad Panamericana, Mexico; Staff Surgeon, Department of Surgery, ABC Hospital, Mexico City; President Sandra Sucar Foundation; Past president Mexican Bord of Specialists in Diseases of Colon and Rectum
Dhatchai Charoesilavath, MD
Associate Professor of Surgery, Chulalongkorn University, Bangkok, Thailand
Colorectal Surgeon, Chulalongkorn Hospital Bangkok, Thailand
USA Faculty
Julia Saraidaridis, MD, FACS, FASCRS
Staff colorectal surgeon in the Division of Colon & Rectal Surgery at Lahey Hospital & Medical Center , Assistant Professor of Surgery at Tufts University School of Medicine; National PI on the BLINQ Study and the ASCRS Anorectal QI Taskforce
Mark K. Soliman, MD, MBA
Chief of Colorectal Surgery and Program Medical Director, AdventHealth Digestive Health Institute; Chair of Colorectal Surgery, AdventHealth Medical Group
Will Perry, MD, MPH
Assistant Professor of Surgery at Mayo Clinic
Colon and rectal surgeon at the Mayo Clinic, Rochester, MN
Honorary Fellow at Oxford University Hospitals NHS Trust
Margarita Murphy, MD
Associate Professor, Florida State University;
Colon and Rectal Surgeon at the Orlando Health Colon and Rectal Institute
Affiliated Assistant Professor, Medical University of South Carolina Medical School
Lilias Maquire, MD
Assistant Professor of Surgery, Perelman School of Medicine, University of Pennsylvania
Colorectal Surgeon, Corporal Michael J. Crescenz Memorial VA Medical Center
Director of Colorectal Research, University of Pennsylvania
Maggie Westfal, MD
Assistant Professor, Medical University of South Carolina
4th Year Medical Student Clerkship Director; Division of Colorectal Surgery Medical University of South Carolina
Stephen Goldstone, MD
Assistant Clinical Professor in Surgery, Icahn School of Medicine at Mount Sinai, New York
Principal Investigator of the ANCHOR Study Group
Jennifer Davids, MD
Section Chief of Colorectal Surgery, Boston Medical Center
Naomi Sell Goldsmith, MD
Colon and Rectal Surgeon at Winchester Hospital, MA
Lillian Chen, MD
Assistant Professor of Surgery, Tufts Medical School
Colon and rectal surgeon at Tufts Medical Center
Angela Khunen, MD
Assistant Professor of Surgery Tufts University School Of Medicine
Colorectal Surgery Fellowship Program Director, Lahey Clinic, MA
David Kleiman, MD
Staff Surgeon, Lahey Hospital and Medical Center
Assistant Professor of Surgery, Tufts University School of Medicine
Thomas Peponis, MD
Assistant Professor of Surgery, Department of Surgery/Division of Colon and Rectal Surgery, UMass Chan Medical School
Jason Hall, MD, MPH
Chairman and Surgeon-in-Chief, Department of Surgery, Tufts Medical Center
Professor and Benjamin Andrews Chair of Surgery, Tufts University School of Medicine
Interim Director, Tufts Medical Center Cancer Center
Olga Beresneva, MD
Assistant Professor of Surgery, Boston University, Chobanian and Avedisian School of Medicine;
Colorectal surgeon at Boston Medical Center
Stanley Goldberg, MD
M Health Fairview Southdale Hospital
University of Minnesota, Minneapolis, MN
Mass General Brigham and Harvard Faculty
Kyle Staller, MD
Associate Professor of Medicine, Harvard Medical School
Director, Gastrointestinal Motility Laboratory at Massachusetts General Hospital
Member, Clinical and Translational Epidemiology Unit at Massachusetts General Hospital
Dana Fugelso, MD
Instructor in Surgery, Harvard Medical School
Beth Israel Deaconess Medical Center
Joel Goldberg, MD
Assistant Professor of Surgery, Harvard Medical School
Brigham and Women's Hospital
Rob Goldstone, MD
Assistant Professor of Surgery, Harvard Medical School
Massachusetts General Hospital
Grace Lee, MD
Assistant Professor of Surgery, Harvard Medical School
Colorectal Surgeon, Massachusetts General Hospital and Salem Hospital
Rich Hodin, MD
Professor of Surgery, Harvard Medical School
Division Chief, Division of Gastrointestinal and Oncologic Surgery, Massachusetts General Hospital
Ron Bleday, MD
Associate Professor of Surgery, Harvard Medical School
Chief, Section Colon and Rectal Surgery, Brigham and Women's Hospital
Vice Chair in Surgery for Quality and Safety
Co-Chair, Mass General Brigham Colorectal Surgery Collaborative
Rocco Ricciardi, MD
Associate Professor of Surgery, Harvard Medical School
Chief, Section Colon and Rectal Surgery, Massachusetts General Hospital
Todd Francone, MD
Associate Professor of Surgery, Tufts Medical School
Division Chief, Colon and Rectal Surgery, Newton Wellesley Hospital
Lieba Savitt, NP-C; WHNP-BC, MSN, MBA
APP Clinical Manager
Division of Gastrointestinal and Oncologic Surgery, Massachusetts General Hospital
Beth O'Dea, NP
Nurse Practitioner, Division of Gastrointestinal and Oncologic Surgery, Massachusetts General Hospital
Hiroko Kunitake, MD
Associate Professor of Surgery, Harvard Medical School
Colorectal Surgery Fellowship Director, Massachusetts General Hospital
Chair, Perioperative Senior Health Clinic, Massachusetts General Hospital
Jonathan Glickman, MD
Associate Professor of Surgery, Harvard Medical School
Holly Bonnette, ANP-BC
Nurse Practitioner, Division of Gastrointestinal and Oncologic Surgery, Massachusetts General Hospital; Lead APP, Colorectal Surgery Center and Center for Pelvic Floor Disorders
Daniel Worrall, ANP-BC
Nurse Practitioner, Division of Gastrointestinal and Oncologic Surgery, Massachusetts General Hospital
Ryan Fong, PA-C
OR Robotics, Brigham and Women's Hospital
Nelya Melnitchouk, MD, MSc
Program Director, Colorectal Surgery Fellowship
Director in Peritoneal Surface Malignancy
Brigham and Women's Hospital
Assistant Professor of Surgery, Harvard Medical School
Accommodations:
W Boston is offering a special group rate for attendees:
- $379.00 USD per night
- Room Type NOT Guaranteed
- Last Day to Book: Wednesday, March 19, 2025
Click here to book your group rate for MGH Colorectal Surgery Course
[format] => full_html ) [field_hotel_link] => Array ( ) [field_hotel_photo] => Array ( ) [field_hotel_travel] => Array ( ) [field_learning_objectives] => Array ( [value] =>Upon completion of this activity, participants will be able to:
- Describe advances in anal fistula, pilonidal cyst, hemorrhoids, and anal fissure management.
- Identify the current controversies in the management of patients with diverticulitis.
- Review the current treatment pathways and appreciate the nuanced surgical options available to patients with inflammatory bowel disease.
- Describe the importance of having multidisciplinary team input to manage complex pelvic floor conditions.
- Discuss international differences in management of benign colorectal diseases and the importance of international exchange of ideas in surgery.
- Practice new technical skills by participating in hands on workshops on a range of procedures including robotic, laparoscopic, anorectal, and high resolution anoscopy.
SUBMIT AN ABSTRACT FOR A POSTER PRESENTATION
The deadline for poster submission is March 1, 2025,
All accepted posters will be scored and judged on Thursday, April 3, 2025 or Friday April 4, 2025 by a panel and will be exhibited electronically throughout the meeting.
| Prizes | |
| 1st Place | $500 + Presentation on Saturday, April 5 + Complimentary Registration for the Main Course, 2026 |
| 2nd Place | $250 + Presentation on Saturday, April 5 + Complimentary Registration for the Main Course, 2026 |
| 3rd Place | $100 + Presentation on Saturday, April 5 + Complimentary Registration for the Main Course, 2026 |
Submission Rules:
- Abstract must be in English, their length must not exceed 3000 characters not including spaces and the headers.
- Abstracts should include : Title, Background, Methods, Results, and Conclusion. The authors and affiliations do not count towards this limit.
- Submission of an abstract requires a paid registration of the first author. Following registration, please email your abstract to lbordeianou@mgh.harvard.edu
- Only one abstract may be submitted per first author. Once received, a confirmation will be sent to the submitting author
- The submitting author is responsible for the content of the abstract and the consent to submit on behalf of all co-authors
Maintenance of Certification (MOC)
American Board of Surgery (ABS) MOC Recognition Statement
Successful completion of this CME activity, which includes participation in the evaluation component, enables the learner to earn credit toward the CME requirement of the American Board of Surgery’s Continuous Certification program. It is the CME activity provider's responsibility to submit learner completion information to ACCME for the purpose of granting ABS credit.
ISUCRS members and Low-Income Country registrants will receive discounted tuition rates. Please use the appropriate code (listed below) at checkout:
ISUCRS Members will receive 15% off when the following code is used: ISUCRS15
Low-Income Country registrants will receive 30% off when the following code is used: LIC30
[format] => full_html ) [field_program] => Array ( [value] =>
Pre-Course Hands-on Workshops (Thursday, April 3)
Option I. Advanced Robotic Colorectal Surgery Hands-On Cadaver Workshop Course Director: Todd Francone, MD (Harvard, USA) Faculty: Thomas Peponis, MD; Will Perry MD; Margarita Murphy, MD; Joel Goldberg, MD; Olga Beresneva, MD A cadaver robotic surgery course that will cover:
|
Option II. Advanced Laparoscopic Surgery Hands-On Cadaver Workshop Course Director: Rocco Ricciardi, MD (Harvard, USA) Faculty: Robert Goldstone, MD; Ayca Gultekin , MD; Lillias Maguire, MD; David Kleiman, MD; Nelya Melnitchouk, MD; Angela Kuhnen, MD A cadaver laparoscopic /open surgery course that will cover:
|
Option III. SOLD OUT - Advanced Anal Fistula and Pilonidal Sinus Surgery Cadaver Hands-On Cadaver Workshop Course Director: Hiroko Kunitake, MD (Harvard, USA) Faculty: Lucia Oliveira, MD; Carlo Ratto, MD; Maggie Westfal, MD; Joseph Nunoo-Mensah, MD; Dhatchai Charoensilavath, MD; Naomi Goldsmith, MD An intensive course on advanced anal fistula repair and pilonidal sinus. We will cover sophisticated anal fistula and pilonidal decision-making though lectures, videos and a hands-on cadaver lab |
Option IV. High Resolution Anoscopy Hands-On WorkshopCourse Directors: Grace Lee, MD and Holly Bonnette, MD (Harvard, USA) Faculty: Danna Fugelso, MD; Daniel Worral, NP; Grace Lee, MD; Holly Bonnette; Lieba Savitt, NP; Lillian Chen, MD; Beth O’Dea NP; Jonathan Glickman Bring yourself and your APP team to improve your familiarity, comfort, and expertise with HRA through lectures, videos, and a hands-on session in a simulation model. |
Main Course: Friday, April 4, 2025 | 7:00am - 5:00pm
| 6:30am | Registration (a light continental breakfast will be served) |
| 7:40 | Welcoming Remarks | Liliana Bordeianou, MD |
| 7:50 | What is the ISUCRS and Why Are We Here | Joseph Nunoo-Mensah, MD (Great Britain) |
Morning Session I: | |
| 8:00am | What Did I Lean on my 4000th Fistula Surgery: Simplified anogenital anatomy and comprehensive anal fistula patterns | Arun Rojanasakul, MD (Thailand) Commentary: Lillias Maguire, MD (USA) |
| 8:20 | Successful Anal Fistula Surgery Benefits from Preoperative Imaging: A Case for Endoanal Ultrasound | Lucia Oliveira, MD (Brazil) |
| 8:30 | Fistulotomy With and Without Immediate Primary Repair | Carlo Ratto, MD (Italy) |
| 8:40 | Why we should stop using setons | Dhatchai Charoensilavath, MD (Thailand) |
| 9:00 | Role and place of VAAFT, FiLAC, Fistura, OTSSC Clip and Fixcision in your Anal Fistula Surgery Arsenal: Serious Procedures or Just Hype ? | Joseph Nunoo-Mensah, MD (Great Britain) |
| 9:10 | Horseshoe Fistula: Now What? | Ayca Gultekin, MD (Turkey) |
| 9:20 | Paul Shellito, MD Lectureship Series - Advanced Anal Fistula Surgery: Partition and Intervention | Introduction by: Hiroko Kunitake, MD Speaker: Arun Rojanasakul, MD (Thailand) Commentary: Stanley Goldberg, MD |
| 9:45 | Panel Discussion |
| 10:20 | Break and Posters Walk Through |
Morning Session II: | |
| 10:30 | Surgery in Patients with Visible External Rectal Prolapse and High-Grade Internal Rectal Intussusception: The European View | Carlo Ratto, MD (Italy) |
| 10:40 | Surgery in Patients with Visible External Rectal Prolapse and High-Grade Internal Rectal Intussusception: The USA View | Liliana Bordeianou, MD (USA) |
| 10:50 | Surgery in Patients with Visible External Rectal Prolapse and High-Grade Internal Rectal Intussusception: The UK View | Joseph Nunoo-Mensah, MD (Great Britain) |
| 11:00 | Recurrent Rectal Prolapse: What Now? | Will Perry, MD (USA) |
| 11:20 | Panel Discussion |
| 11:50 | Break |
Morning Session III: | |
| 12:00pm | Anal Fissure: BLINQ, Please | Julia Saraidaridis, MD (USA) |
| 12:10 | Hemorrhoids : Anything New To Offer Since WWII | Gonzalo Hagerman, MD (Mexico) |
| 12:20 | Complex Pilonidal Diseases: My Favorite Flaps, How I Do Them, and Why | Margarita Murphy, MD (USA) |
| 12:30 | Panel Discussion |
| 1:00 | Lunch (complimentary) and Poster Walk Through |
Afternoon Session I: | |
| 2:00 | Why Did I Get Diverticulitis and Can I Prevent it From Coming Back? | Julia Saraidaridis, MD (USA) |
| 2:10 | Should We Stop Giving Antibiotics to Admitted Patients with Diverticulitis: Lessons from the STAND, AVOD and DIABOLO trials | Thomas Peponis, MD (USA) |
Debate: When To Operate on Patients With Recurrent Diverticulitis | |
| 2:20 | Setting the Debate Scene: Patient Focused Decision Making in Diverticulitis. How to Decide Who Benefits from an Elective Sigmoid Colectomy? | Jason Hall, MD (USA) |
| 2:35 | Arguments for Prompt Surgery: “Enough Already! Just Take The Colon O-U-T OUT!” | Joseph Nunoo- Mensah, MD (Great Britain) |
| 2:50 | Arguments for Medical Therapy: “ There are Many Effective Strategies to Prevent Recurrent Diverticulitis: First, Do No Harm” | Lillias Maguire, MD (USA) |
| 3:05 | Rebuttal | Joseph Nunoo-Mensah, MD (Great Britain) |
| 3:10 | Rebuttal | Lillias Maguire, MD (USA) |
| 3:15 | Discussion, Vote, and Crowning of Winner |
Afternoon Session II | |
| 3:20 | Robotic Sigmoid Resection for Complicated Diverticulitis : Key Technical Points To Master As You Progress On Your Learning Curve | Mark Soliman, MD (USA) |
| 3:40 | How Long Can One Sit on a Stable Patient with Perforated Diverticulitis – and Does it Make Sense to Do It? | Thomas Peponis (USA) |
| 3:50 | Goodbye, Hartman or Not Quite Yet? | Gabriela Möslein, MD (Germany) |
| 4:00 | Panel Discussion |
| 5:00pm | Adjourn |
Main Course: Saturday, April 5, 2025 | 7:00am - 5:00pm
| 7:00am | Breakfast |
Morning Session I: | |
| 8:00am | Primer on IBD Meds for the Surgeon: What to Hold and What to Keep Preop and Postop | David Kleiman, MD (USA) |
| 8:10 | Surgical Bailouts for a Technically Challenging IPAA: Know Your Options | Jennifer Davids, MD (USA) |
| 8:30 | Ernest Codman Lectureship Series: Is Continent Ileostomy In or Out of Fashion Again? Introduction by: Christy Cauley, MD Speaker: Gabriela Möslein, MD (Germany) |
| 9:00 | Segmental or Total Colectomy in UC patients with Dysplasia: Do We Have Any Data for a Rational Decision | Richard Hodin, MD (USA) |
| 9:10 | Ileocecal Resection with Various Anastomotic Techniques | Maggie Westfal, MD (USA) |
| 9:20 | Does Diversion Have a Place in A Patient with Ileocecal Crohn’s? | Will Perry, MD |
| 9:30 | Approaching the Patient with Fistulizing Crohn’s Disease | Joel Goldberg, MD (USA) |
| 9:40 | Panel Discussion |
| 10:15 | Break |
Morning Session II: | |
| 10:30 | Parastomal Hernia | Rob Goldstone, MD (USA) |
| 10:40 | My Colonic Conduit is Dead/Does Not Reach? | Marc Soliman, MD (USA) |
| 10:50 | Lower GI Bleeding | Joseph Nunoo-Mensah, MD (Great Britain) |
| 11:00 | Stapler Does Not Fit or Pass Through a Kink | Olga Beresneva, MD (USA) |
| 11:10 | Anastomotic Leak | Rocco Ricciardi, MD (USA) |
| 11:20 | Challenging Stoma | Lucia Oliveira, MD (Brazil) |
| 11:30 | Ghost Ileostomy vs. Early Ileostomy Closure: Which Approach Makes More Sense To Me? | Lilian Chen, MD (Germany) |
| 11:40 | Postoperative Ileus | Grace Lee, MD (USA) |
| 11:50 | Is Surgery for Slow Transit Constipation Still A Thing? | Kyle Staller, MD (USA) |
| 12:00pm | Obstetric Anal Sphincter Injury | Carlo Ratto, MD (Italy) |
| 12:10 | On Rectovaginal Fistula and Other Surgical Principles Re-Learned During My Missions in Africa | Gonzalo Hagerman, MD (Mexico) |
| 12:20 | Is There New Hope for Fecal Incontinence Patients? | Margarita Murphy, MD (USA) |
| 12:30 | Panel Discussion |
| 1:00 | Lunch (complimentary) |
Afternoon Session: | |
| 2:00 | Anal Fistula: My Favorite Approach | Carlo Ratto, MD (Italy) |
| 2:10 | Anal Fistula: My Favorite Approach | Dhatchai Charoensilavath, MD (Thailand) |
| 2:20 | Anal Fistula: My Favorite Approach | Joseph Nunoo-Mensah, MD (Great Britain) |
| 2:30 | Anal Fistula: My Favorite Approach | Lucia Oliveira, MD (Brazil) |
| 2:40 | Pilonidal Cyst: Treatment Depends on Its Grade | Will Perry, MD (USA) |
| 2:50 | Pilonidal Cyst: My Favorite Approach | Ayca Gultekin, MD (Turkey) |
| 3:20 | Useful Intra- Op Tricks: Using ICG to Your Patient’s Advantage | Olga Beresneva, MD (USA) |
| 3:30 | Rectal Prolapse: My Favorite Approach | Liliana Bordeianou, MD (USA) |
| 3:40 | Intraoperative Emergency: Stay Calm | Todd Francone, MD (USA) |
| 3:50 | Intraoperative Emergency: Stay Calm | Marc Soliman, MD (USA) |
| 4:00 | Poster Competition Winner: First Place | TBD |
| 4:10 | Poster Competition Winner: Second Place | TBD |
| 4:20 | Poster Competition Winner: Third Place | TBD |
| 4:30 | Discussion, Closing Remarks | Rocco Ricciardi, MD (USA) |
| 5:00pm | Adjourn |
Please Note: The Anal Fistula/Pilonidal Cadaver Workshop is SOLD OUT
ISUCRS members and Low-Income Country registrants will receive discounted tuition rates. Please use the appropriate code (listed below) at checkout:
ISUCRS Members will receive 15% off when the following code is used: ISUCRS15
Low-Income Country registrants will receive 30% off when the following code is used: LIC30
Thursday Hands On Workshops ONLY (In-Person):
| Hands-On Workshop ONLY | Early Bird (ends March 1) | After March 1 |
|---|---|---|
(MD, NP, PA, Students, Fellows)
| $1150.00 | $1250.00 |
| HRA Hands-On Workshop | ||
| MD | $125.00 | $150.00 |
| NP, PA | $80.00 | $100.00 |
| Students & Fellows | $5.00 | $5.00 |
Friday & Saturday Main Course ONLY (In-Person or Virtual):
| Tuition Type | Early Bird (ends March 1) | After March 1 |
|---|---|---|
| MD | $400.00 | $450.00 |
| NP, PA | $300.00 | $350.00 |
| Students & Fellows (In-Person) | $35.00 | $50.00 |
| Students & Fellows (Virtual) | $5.00 | $5.00 |
Thursday Workshop AND Friday/Saturday Main Course:
| Tuition Type | Early Bird (ends March 1) | After March 1 |
|---|---|---|
Main Course AND Hands-On Workshop (Thu-Sat)
| $1350.00 | $1400.00 |
Main Course AND HRA Lab Combo (Thu-Sat) - MD | $450.00 | $500.00 |
| Main Course AND HRA Lab Combo (Thu-Sat) - NP, PA | $350.00 | $400.00 |
| Main Course AND HRA Lab Combo (Thu-Sat) - Students & Fellows | $35.00 | $50.00 |
Cancellation Policy:
Registrations cancelled on or before March 20, 2025 will be refunded, less a $50 administrative fee. Registrations cancelled after March 20, 2025 will not be refunded.
Contact mgbcpd@mgb.org if you require assistance in cancelling your online registration.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for general surgeons, colorectal surgeons, gastroenterologists, urogynecologists, nurse practitioners, physician assistants, nurses, and students.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3598 [id] => 3598 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital, a teaching affiliate of Harvard Medical School in collaboration with the International Society of University Colorectal Surgeons (ISUCRS) and Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=85178
[first] => https://cpd.partners.org/node?nid=85178&page=0
[last] => https://cpd.partners.org/node?nid=85178&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, this activity has been planned and implemented by Mass General Brigham and Cambial Healthcare Consulting, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team
Mass General Brigham designates this live activity for a maximum of 5.00 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1750442400
[value2] => 1785297540
[duration] => 34855140
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/88970
[id] => 88970
[resource] => file
[uuid] => 5a7ef150-6979-48ed-be62-2c4d9e6134c4
)
)
[field_course_intro] => Array
(
)
[field_course_live] =>
[field_course_location] => Array
(
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => This is a live, in-person activity
Amid ongoing changes and growing uncertainty in the healthcare landscape, it's more important than ever to pause & reflect on what success truly means to you - and how best to achieve it. Our day-long, small-group retreats are designed specifically for mid-career physicians and leaders in medicine. Through expert facilitation, participants are guided in evaluating their goals and developing intentional strategies. Held in-person at off-site locations, these retreats offer a focused environment free from the distractions of daily routines, creating the space needed for meaningful reflection & planning.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Emily Hayden, MD, MHPE - Course Director
Director of Telehealth, Department of Emergency Medicine - Massachusetts General Hospital
Director of Emergency Medicine Telehealth Research Lab, Division of Health Services Research - Mass General Brigham
Associate Professor of Emergency Medicine, Harvard Medical School
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Describe their individual career assumptions.
- Evaluate the accuracy of their career believes and modify inaccurate beliefs.
- Write a near- and longer-term vision of success for their career.
[format] => full_html
)
[field_program] => Array
(
)
[field_registration_instructions] => Array
(
)
[field_related_courses] => Array
(
)
[field_requirements_max] =>
[field_requirements_min] =>
[field_show_child_catalog] =>
[field_show_child_transcript] =>
[field_target_audience] => Array
(
[value] => This activity is intended for mid-career physicians and leaders in medicine.
[format] => full_html
)
[field_venue_phone] => Array
(
)
[upload] => Array
(
)
[field_accme_data] => Array
(
[uri] => https://cpd.partners.org/accme_data/3886
[id] => 3886
[resource] => accme_data
)
[field_show_on_calendar] =>
[field_custom_provided] => Array
(
[value] => Massachusetts General Hospital, Cambial Healthcare Consulting & Mass General Brigham
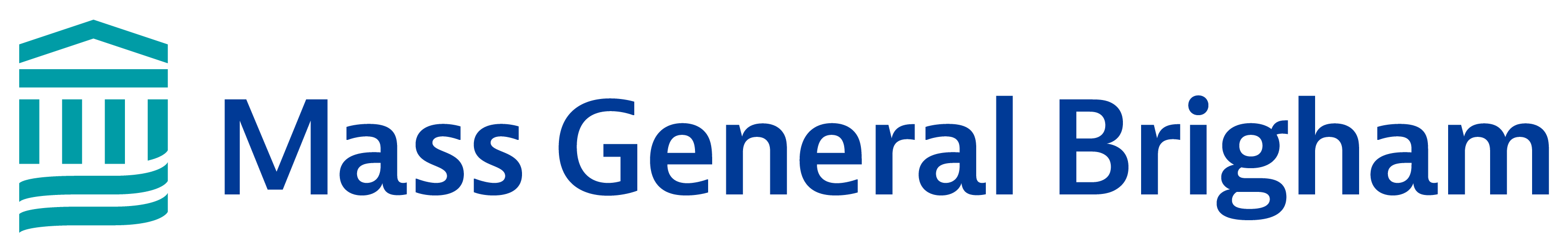
[summary] =>
[format] => full_html
)
[field_course_exhibitor] => Array
(
)
[field_course_qualifiers] => Array
(
)
[field_course_image_cards] => Array
(
)
[field_income_expense] => Array
(
)
[og_membership] => Array
(
)
[og_membership__1] => Array
(
)
[og_membership__2] => Array
(
)
[og_membership__3] => Array
(
)
[og_group_ref__og_membership] => Array
(
)
[og_group_ref__og_membership__1] => Array
(
)
[og_group_ref__og_membership__2] => Array
(
)
[og_group_ref__og_membership__3] => Array
(
)
[flag_course_bookmark_user] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/user/34225
[id] => 34225
[resource] => user
[uuid] => b8439059-f1bb-4b19-878a-d8f32cab11b7
)
[1] => Array
(
[uri] => https://cpd.partners.org/user/165375
[id] => 165375
[resource] => user
[uuid] => 70ba7226-b27d-40ef-afb4-5907f84023e6
)
)
[model] => course_85178
[list_price] => 0.00000
[cost] => 0.00000
[sell_price] => 0.00000
[price] => 0.00000
[weight] => 0
[weight_units] => lb
[length] => 0
[width] => 0
[height] => 0
[length_units] => in
[pkg_qty] => 1
[ordering] => 0
[shippable] => 0
[nid] => 85178
[vid] => 232294
[is_new] =>
[type] => course
[title] => Career Restoration Retreats 2025-2026
[language] => und
[url] => https://cpd.partners.org/content/career-restoration-retreats-2025-2026
[edit_url] => https://cpd.partners.org/node/85178/edit
[status] => 1
[promote] => 0
[sticky] => 0
[created] => 1750444475
[changed] => 1751043420
[author] => Array
(
[uri] => https://cpd.partners.org/user/316
[id] => 316
[resource] => user
[uuid] => d6db325c-6680-48ed-a601-f114e3fb592a
)
[log] =>
[revision] =>
[course] => Array
(
[uri] => https://cpd.partners.org/course/85178
[id] => 85178
[resource] => course
)
[book_ancestors] => Array
(
)
[comment] => 1
[comments] => Array
(
)
[comment_count] => 0
[comment_count_new] => 0
[body] => Array
(
)
[feeds_item_guid] =>
[feeds_item_url] =>
[feed_nid] =>
[relation_faculty_user] => Array
(
)
[uuid] => 3d6a6fcc-24f9-4e75-a42a-15f7dd2d6fe8
[vuuid] => ed578f55-6ab1-4336-aca6-525892e7ff7d
)
)
)
Array
(
[self] => https://cpd.partners.org/node?nid=70270
[first] => https://cpd.partners.org/node?nid=70270&page=0
[last] => https://cpd.partners.org/node?nid=70270&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this live activity for a maximum of 13.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 13.5 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
Please note: up to 13.5 credits will be awarded if you attend both the symposium AND Immunotherapy Toxicities optional session.
If you attend the symposium only, you will be awarded up to 11.5 credits.
If you attend the Immunotherapy Toxicities optional session only, you will be awarded up to 2 credits.
MOC Recognition Statement
Successful completion of this CME activity, which includes participation in the activity, with individual assessments of the participant and feedback to the participant, enables the participant to earn 13.5 MOC points in the American Board of Internal Medicine (ABIM) Maintenance of Certification (MOC) program. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
Please note: up to 13.5 MOC points will be awarded if you attend both the symposium AND Immunotherapy Toxicities optional session.
If you attend the symposium only, you will be awarded up to 11.5 MOC points.
If you attend the Immunotherapy Toxicities optional session only, you will be awarded up to 2 MOC points.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/231
[id] => 231
[resource] => taxonomy_term
[uuid] => 541dec03-c6af-4bcb-9af7-8fa28fedfb53
)
[1] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/244
[id] => 244
[resource] => taxonomy_term
[uuid] => 41b0f6bc-954e-439d-b355-009eb871e393
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1710958020
[value2] => 1734325140
[duration] => 23367120
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1731587400
[value2] => 1731703800
[duration] => 116400
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/238
[id] => 238
[resource] => taxonomy_term
[uuid] => fd81c17a-d19b-46b8-ad6b-2c5aee9ce9be
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/65480
[id] => 65480
[resource] => file
[uuid] => 9d4255a7-c916-49bd-ab9c-8e15c95e9b41
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 50623
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Joseph B. Martin Conference Center
[street] => 77 Avenue Louis Pasteur
[additional] =>
[city] => Boston
[province] => MA
[postal_code] => 02115
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => Please Note:
This course has two components you can register for. You can either register for the symposium only, Immunotherapy Toxicities session only, or both
Cancer treatment has evolved significantly over the past decade from a treatment paradigm anchored on surgery, chemotherapy, and radiotherapy, to one embracing molecularly-targeted therapies disrupting tumor-specific signaling pathways, as well as new approaches to mobilize the immune system. For clinicians trying to keep current with advancing immuno-oncology principles and research, the pace of these developments has brought new challenges. Recognizing these challenges, this course will provide a comprehensive clinical review of the advances taking place in the immuno-oncology field.
This year we have added an optional session on Immunotherapy Toxicities, focusing on the identification and management of common and uncommon toxicities from immune-checkpoint inhibitors. Attendance at this session, entitled “Sink or Swim: Navigating the Murkey Waters of Immunotherapy Toxicities” is optional and available for an additional fee. It will take place after the close of the general session on the second day. Attendance at the Advances in Cancer Immunotherapy symposium is NOT required to attend this toxicities session, you may register to ONLY attend this part of the program.
| Registration Type | Symposium Tuition Fee | Symposium AND Afternoon Toxicities Session Tuition Fee |
|---|---|---|
| Physicians | $199.00 | $235.00 |
| Fellows/Nurses/PAs/etc. | $99.00 | $135.00 |
| Industry | $499.00 | $549.00 |
| Afternoon Toxicities Session ONLY | N/A | $50.00 |
Course Directors
Justin Gainor, MD
Director, Center for Thoracic Cancers,
Director of Targeted Immunotherapy,
Massachusetts General Hospital Cancer Center;
Associate Professor of Medicine, Harvard Medical School
Krista Rubin, MS, FNP-BC
Nurse Practitioner, Center for Melanoma,
Massachusetts General Hospital Cancer Center
Ryan Sullivan, MD
Physician Investigator, Cancer Center, Mass General Research Institute;
Assistant In Medicine, Hematology-Oncology, Massachusetts General Hospital;
Associate Professor of Medicine, Harvard Medical School
Faculty
Steven Blum, MD
Instructor in Medicine,
Massachusetts General Hospital
Priscilla Brastianos, MD
Associate Professor of Medicine, Harvard Medical School;
Physician Investigator, Mass General Research Institute;
Assistant Physician, Massachusetts General Hospital Cancer Center
Daniel P. Cahill, MD, PhD
Professor of Neurosurgery, Harvard Medical School;
Neurosurgical Oncologist, Department of Neurosurgery,
Massachusetts General Hospital
Michael Dougan, MD, PhD
Massachusetts General Hospital
Riley Fadden, MSN, RN, FNP-C
Nurse Practitioner, Center for Melanoma,
Massachusetts General Hospital Cancer Center
Alexander Faje, MD
Massachusetts General Hospital
Christine Freedman, RN
Massachusetts General Hospital Cancer Center
Xin Gao, MD
Assistant in Medicine, Massachusetts General Hospital Cancer Center;
Assistant Professor, Harvard Medical School
Elizabeth Gerstner, MD
Associate Professor of Neurology, Harvard Medical School;
Department of Neurology, Massachusetts General Hospital
Amanda Guidon, MD, MPH
Massachusetts General Hospital
Rakesh Jain, PhD
Director, Steele Laboratory, Massachusetts General Hospital;
A. Werk Cook Professor of Radiation Oncology, Harvard Medical School
Howard Kaufman, MD
Assistant in Surgery, Surgery, Massachusetts General Hospital;
Lecturer in Surgery, Harvard Medical School
Florence (Katie) Keane, MD
Assistant Professor in Radiation Oncology,
Massachusetts General Hospital
Meghan Mooradian, MD
Instructor, Medicine, Harvard Medical School;
Clinical Oncologist, Medial Oncology,
Massachusetts General Hospital Cancer Center
Iman Osman, MD
Rudolf L. Baer Professor of Dermatology,
Ronald O. Perelman Department of Dermatology,
Professor, Department of Medicine,
Professor, Department of Urology,
NYU Langone Health
Patrick Ott, MD, PhD
Clinical Director, Melanoma Disease Center,
Director, Clinical Sciences, Center for Immuno-Oncology,
Dana-Farber Cancer Institute;
Associate Professor of Medicine, Harvard Medical School
Jong Chul Park, MD
Assistant Professor of Medicine,
Massachusetts General Hospital Cancer Center
Michael Parsons, PhD
Associate Professor of Psychology, Harvard Medical School;
Neuropsychologist, Pappas Neuro-Oncology Center, Department of Psychiatry,
Massachusetts General Hospital
Laura Petrillo, MD
Palliative Care Physician, Massachusetts General Hospital;
Assistant Professor of Medicine, Harvard Medical School
Kerry Reynolds, MD
Clinical Director, Inpatient Oncology Units,
Director, Severe Immunotherapy Complications Program,
Massachusetts General Hospital Cancer Center
Sherin J. Rouhani, MD, PhD
Inpatient Oncologist,
Massachusetts General Hospital Cancer Center
Kurt Schalper, MD, PhD
Associate Professor of Pathology,
Director, Translational Immuno-oncology Laboratory,
Yale School of Medicine
Arlene Sharpe, MD, PhD
Kolokotrones University Professor,
Chair, Department of Immunology,
Harvard Medical School
Nathaniel Treister, DMD, DMSc
Brigham & Women’s Hospital
Alexandra-Chloe Villani, PhD
Director, Single-Cell Genomics Program,
Center for Immunology and Inflammatory Diseases,
Massachusetts General Hospital;
Assistant Professor of Medicine, Harvard Medical School;
Associate Scientist, Broad Institute of MIT and Harvard
Oladapo Yeku, MD, PhD, FACP
Physician Investigator, Mass General Research Institute;
Assistant Professor of Medicine, Harvard Medical School;
Assistant in Medicine, Massachusetts General Hospital Cancer Center
Accommodations
A limited number of rooms have been held at the Boston Marriott Copley Place for the nights of November 13, 14, and 15 at a rate of $279.00 per night. To book a room in the block, please click HERE or call the hotel directly at 1-800-228-9290. The deadline to book is Wednesday, October 23, 2024.
[format] => full_html ) [field_hotel_link] => Array ( ) [field_hotel_photo] => Array ( ) [field_hotel_travel] => Array ( ) [field_learning_objectives] => Array ( [value] =>Upon completion of this activity, participants will be able to:
- Evaluate cancer immunotherapy principles and strategies and how they influence current treatment approaches.
- Identify the emerging role of personalized cancer vaccination and other immunotherapy combinations in patients with solid tumor and hematologic malignancies.
- Define currently approved and emerging predictive biomarkers for cancer immunotherapy.
- Recognize and implement management strategies for immune-mediated side effects in patients treated with immunotherapy agents.
- Recognize the importance of establishing a multidisciplinary approach in the immunotherapy era.
For exhibit space, please contact ebrooks3@mgb.org
MEDICAL EDUCATION GRANT DISCLOSURE
Advances in Cancer Immunotherapy 2024: Annual Update has received support in the form of educational grants from Bristol Myers Squibb and Regeneron.
[format] => full_html ) [field_program] => Array ( [value] =>Thursday, November 14, 2024 | 7:30am - 4:00pm
7:30 am | Registration and Breakfast* |
8:00 | Welcome | Justin Gainor, MD; Krista Rubin, MS, FNP-BC; Ryan Sullivan, MD |
8:05 | Primer | Howard L. Kaufman, MD |
8:35 | Q&A |
8:45 | Overview of Immunology Tolerance | Arlene Sharpe, MD, PhD |
9:15 | Q&A |
9:25 | Cancer Immunotherapy: Where are We Now? | Justin Gainor, MD |
9:55 | Q&A |
| 10:05 | BREAK* |
10:20 | Cellular Therapies Lecture | Oladapo Yeku , MD, PhD, FACP |
10:50 | Q&A |
11:00 | Normalizing the Tumor Microenvironment to Improve Cancer Immunotherapy: Bench to Bedside | Rakesh Jain, PhD |
11:30 | Q&A |
| 11:40 | RAPID FIRE!!! Cancer Immunotherapy for the Non-Medical Oncologist Panelists:
|
12:10pm | LUNCH* |
1:00 | Debate: When, If Ever, to Stop Immunotherapy | Meghan Mooradian, MD & Xin Gao, MD |
1:30 | Q&A |
1:40 | Mechanisms of Immunotherapy Toxicity | Alexandra-Chloe Villani, PhD |
2:10 | Q&A |
2:20 | BREAK* |
2:35 | Toxicity – Clinical and Practical | Kerry Reynolds, MD & Krista Rubin, MS, FNP-BC |
3:05 | Q&A |
3:15 | Interactive Case Studies | Steve Blum, MD & Sherin Rouhani, MD, PhD |
| 4:00 pm | Closing Remarks and Adjourn |
*The exhibit hall will be open during breakfast, breaks, and lunch
Friday, November 15, 2024 | 7:30am - 1:00pm
Optional Toxicities Session: 1:30pm - 3:50pm
7:30 am | Registration and Breakfast* |
8:00 | Welcome | Justin Gainor, MD; Krista Rubin, MS, FNP-BC; Ryan Sullivan, MD |
8:05 | Predicting Response and Toxicity to Immune Check Point Inhibition: Is There a Simple (but Not Simplistic) Way | Iman Osman, MD |
| 8:35 | Q&A |
8:45 | Biomarkers Debate: Blood vs. Tissue | |
9:15 | Q&A |
9:25 | Incorporating Biomarker Analysis into Optimal Treatment Selection | Kurt Schalper, MD, PhD |
9:55 | Q&A |
| 10:05 | BREAK* |
10:20 | Balancing the Risks & Benefits of Peri/Post-Operative Immunotherapy | Ryan Sullivan, MD |
| 10:50 | Q&A |
11:00 | Panel Discussion: Incorporating Checkpoint Inhibitors into Multidisciplinary Brain Metastases Care | |
12:00 pm | RAPID FIRE!!! What’s Next in Immunotherapy?
|
12:30 | Q&A |
12:40 | Wrap-Up Session | Justin Gainor, MD; Krista Rubin, MS, FNP-BC; Ryan Sullivan, MD |
1:00 pm | Adjourn |
*The exhibit hall will be open during breakfast, breaks, and lunch
Sink or Swim: Navigating the Murky Waters of Immunotherapy Toxicities
Identification and management of common and uncommon toxicities from immune-checkpoint inhibitors
1:30 pm | Introduction | Krista Rubin, MS, FNP-BC |
1:35 | Endocrine Toxicities | Alexander Faje, MD |
| 1:55 | Q&A |
2:05 | Oral Toxicities | Nathaniel Treister, DMD, DMSc |
2:25 | Q&A |
2:35 | BREAK |
2:45 | NeuroMuscular Toxicities | Amanda Guidon, MD, MPH |
| 3:05 | Q&A |
3:15 | Gastrointestinal Toxicities | Michael Dougan, MD, PhD |
| 3:35 | Q&A |
3:40 | Closing Remarks | Krista Rubin, MS, FNP-BC |
3:50 pm | Adjourn |
| Registration Type | Symposium Tuition Fee | Symposium AND Afternoon Toxicities Session Tuition Fee |
|---|---|---|
| Physicians | $199.00 | $235.00 |
| Fellows/Nurses/PAs/etc. | $99.00 | $135.00 |
| Industry | $499.00 | $549.00 |
| Afternoon Toxicities Session ONLY | N/A | $50.00 |
Cancellation Policy:
Registrations cancelled on or before October 31, 2024 will be refunded, less a $35 administrative fee. Registrations cancelled after October 31, 2024 will not be refunded.
Contact partnerscpd@partners.org if you require assistance in cancelling your online registration.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for physicians, nurses, physician assistants, and other members of the healthcare team.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3179 [id] => 3179 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital Cancer Center & Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=84839
[first] => https://cpd.partners.org/node?nid=84839&page=0
[last] => https://cpd.partners.org/node?nid=84839&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statement
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this enduring material for a maximum of 14.00 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Maintenance of Certification (MOC)
American Board of Surgery (ABS) MOC Recognition Statement
Successful completion of this CME activity, which includes participation in the evaluation component, enables the learner to earn credit toward the CME requirement of the American Board of Surgery’s Continuous Certification program. It is the CME activity provider’s responsibility to submit learner completion information to ACCME for the purpose of granting ABS credit.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/540
[id] => 540
[resource] => taxonomy_term
[uuid] => e731fa5e-224d-48ef-a2bf-def1293fa566
)
[1] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/539
[id] => 539
[resource] => taxonomy_term
[uuid] => 57fa07dc-bb22-48eb-bff3-97c75764b9e6
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1749211200
[value2] => 1780718340
[duration] => 31507140
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/237
[id] => 237
[resource] => taxonomy_term
[uuid] => 842d3b08-d27d-4a11-8281-71bcfb00ec51
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/77642
[id] => 77642
[resource] => file
[uuid] => 44fa0bec-301e-4e67-a94c-411d284e71db
)
)
[field_course_intro] => Array
(
)
[field_course_live] =>
[field_course_location] => Array
(
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => Please Note: This is the enduring version of the live course that took place in April 2025

Harvard Medical School (HMS) faculty and renowned national and international experts from the International Society of University Colon and Rectal Surgeons (ISUCRS) reviewed the latest advancements in surgical treatments for benign diseases of the colon and rectum.
The event featured updates from world-class surgeons from around the globe, including Dr. Joseph Nunoo Mensah (UK), Dr. Lucia Oliveira (Brazil), Dr. Carlo Ratto (Italy), Dr. Ayca Gultekin (Turkey), Dr. Gonsalo Hagerman (Mexico), and many others. The lectures were enhanced with videos and interactive content, offering participants a comprehensive learning experience.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Course Directors
Liliana Bordeianou, MD
Professor of Surgery, Harvard Medical School;
Co-Director, MGH Pelvic Floor Disorders Center,
Co-Chair, Mass General Brigham Colorectal Surgery Collaborative,
Massachusetts General Hospital
Christy Cauley, MD
Assistant Professor Harvard Medical School;
Colorectal Surgeon, Gastrointestinal Surgeon
Massachusetts General Hospital
International Faculty
Joseph Nunoo Mensah, MD, FASCRS
Colorectal Surgeon at Kings College Hospital and Cleveland Clinic London,UK; Head of the Department of Colorectal Surgery; Former President of the International Society of University Colon and Rectal Surgeons (ISUCRS) from 2022-24.
Arun Rojanasakul, MD, FASCRS
Emeritus Prof at the Banpakok International Hospital in Bangkok, Thailand: Honorary FASCRS (USA), PSCS (Phillipines), ACRSI (India) and SSCS (Singapore) Fellow; Past president of the Colorectal Surgery Committee of Thailand and the Coloproctology Association of Asia-Pacific; Inventor of the LIFT (Ligation Intersphincteric Fistula Tract) Procedure
Lucia Oliveira, MD
Director of the Anorectal Physiology department, Cepemed, Rio de Janeiro, Brazil; Board Member of ALAPP (Latin American Pelvic Floor Society)
Carlo Ratto, MD, FASCRS
Prof. Ratto is the Chief of the Unit of Proctology and Pelvic Floor Surgery at the Isola Tiberina Gemelli Hospital in Rome, Italy, and Hon FASCRS (USA)
Ayca Gultekin, MD
Professor of Surgery, Zonguldak Bulent Ecevit University School of Medicine, Turkey; Editor in Chief, Turkish Journal of Colorectal Disease; Assistant Secretary, UEMS (European Union of Medical Specialists) Section of Surgery-Coloproctology; Chair of Pelvic Floor Disorders Group, Turkish Society of Colon and Rectal Surgery
Gabriela Möslein, MD
Professor of Surgery and Dept. Head of the newly established Center for Hereditary Tumors at the Academic Hospital of the University of Düsseldorf Ev. BETHESDA in Duisburg, Germany;
Director of InSiGHT (International Society for Hereditary Gastrointestinal Tumors)
Former Secretary of ESCP (European Society for Coloproctology) from 2016 – 2020 and ESCP Program Director(2020-2024)
Gonzalo Hagerman, MD , FASCRS
Professor, Universidad Panamericana, Mexico; Staff Surgeon, Department of Surgery, ABC Hospital, Mexico City; President Sandra Sucar Foundation; Past president Mexican Bord of Specialists in Diseases of Colon and Rectum
Dhatchai Charoesilavath, MD
Associate Professor of Surgery, Chulalongkorn University, Bangkok, Thailand
Colorectal Surgeon, Chulalongkorn Hospital Bangkok, Thailand
USA Faculty
Julia Saraidaridis, MD, FACS, FASCRS
Staff colorectal surgeon in the Division of Colon & Rectal Surgery at Lahey Hospital & Medical Center , Assistant Professor of Surgery at Tufts University School of Medicine; National PI on the BLINQ Study and the ASCRS Anorectal QI Taskforce
Mark K. Soliman, MD, MBA
Chief of Colorectal Surgery and Program Medical Director, AdventHealth Digestive Health Institute; Chair of Colorectal Surgery, AdventHealth Medical Group
Will Perry, MD, MPH
Assistant Professor of Surgery at Mayo Clinic
Colon and rectal surgeon at the Mayo Clinic, Rochester, MN
Honorary Fellow at Oxford University Hospitals NHS Trust
Margarita Murphy, MD
Associate Professor, Florida State University;
Colon and Rectal Surgeon at the Orlando Health Colon and Rectal Institute
Affiliated Assistant Professor, Medical University of South Carolina Medical School
Lilias Maquire, MD
Assistant Professor of Surgery, Perelman School of Medicine, University of Pennsylvania
Colorectal Surgeon, Corporal Michael J. Crescenz Memorial VA Medical Center
Director of Colorectal Research, University of Pennsylvania
Maggie Westfal, MD
Assistant Professor, Medical University of South Carolina
4th Year Medical Student Clerkship Director; Division of Colorectal Surgery Medical University of South Carolina
Stephen Goldstone, MD
Assistant Clinical Professor in Surgery, Icahn School of Medicine at Mount Sinai, New York
Principal Investigator of the ANCHOR Study Group
Jennifer Davids, MD
Section Chief of Colorectal Surgery, Boston Medical Center
Naomi Sell Goldsmith, MD
Colon and Rectal Surgeon at Winchester Hospital, MA
Lillian Chen, MD
Assistant Professor of Surgery, Tufts Medical School
Colon and rectal surgeon at Tufts Medical Center
Angela Khunen, MD
Assistant Professor of Surgery Tufts University School Of Medicine
Colorectal Surgery Fellowship Program Director, Lahey Clinic, MA
David Kleiman, MD
Staff Surgeon, Lahey Hospital and Medical Center
Assistant Professor of Surgery, Tufts University School of Medicine
Thomas Peponis, MD
Assistant Professor of Surgery, Department of Surgery/Division of Colon and Rectal Surgery, UMass Chan Medical School
Jason Hall, MD, MPH
Chairman and Surgeon-in-Chief, Department of Surgery, Tufts Medical Center
Professor and Benjamin Andrews Chair of Surgery, Tufts University School of Medicine
Interim Director, Tufts Medical Center Cancer Center
Olga Beresneva, MD
Assistant Professor of Surgery, Boston University, Chobanian and Avedisian School of Medicine;
Colorectal surgeon at Boston Medical Center
Stanley Goldberg, MD
M Health Fairview Southdale Hospital
University of Minnesota, Minneapolis, MN
Mass General Brigham and Harvard Faculty
Kyle Staller, MD
Associate Professor of Medicine, Harvard Medical School
Director, Gastrointestinal Motility Laboratory at Massachusetts General Hospital
Member, Clinical and Translational Epidemiology Unit at Massachusetts General Hospital
Dana Fugelso, MD
Instructor in Surgery, Harvard Medical School
Beth Israel Deaconess Medical Center
Joel Goldberg, MD
Assistant Professor of Surgery, Harvard Medical School
Brigham and Women's Hospital
Rob Goldstone, MD
Assistant Professor of Surgery, Harvard Medical School
Massachusetts General Hospital
Grace Lee, MD
Assistant Professor of Surgery, Harvard Medical School
Colorectal Surgeon, Massachusetts General Hospital and Salem Hospital
Rich Hodin, MD
Professor of Surgery, Harvard Medical School
Division Chief, Division of Gastrointestinal and Oncologic Surgery, Massachusetts General Hospital
Ron Bleday, MD
Associate Professor of Surgery, Harvard Medical School
Chief, Section Colon and Rectal Surgery, Brigham and Women's Hospital
Vice Chair in Surgery for Quality and Safety
Co-Chair, Mass General Brigham Colorectal Surgery Collaborative
Rocco Ricciardi, MD
Associate Professor of Surgery, Harvard Medical School
Chief, Section Colon and Rectal Surgery, Massachusetts General Hospital
Todd Francone, MD
Associate Professor of Surgery, Tufts Medical School
Division Chief, Colon and Rectal Surgery, Newton Wellesley Hospital
Lieba Savitt, NP-C; WHNP-BC, MSN, MBA
APP Clinical Manager
Division of Gastrointestinal and Oncologic Surgery, Massachusetts General Hospital
Beth O'Dea, NP
Nurse Practitioner, Division of Gastrointestinal and Oncologic Surgery, Massachusetts General Hospital
Hiroko Kunitake, MD
Associate Professor of Surgery, Harvard Medical School
Colorectal Surgery Fellowship Director, Massachusetts General Hospital
Chair, Perioperative Senior Health Clinic, Massachusetts General Hospital
Jonathan Glickman, MD
Associate Professor of Surgery, Harvard Medical School
Holly Bonnette, ANP-BC
Nurse Practitioner, Division of Gastrointestinal and Oncologic Surgery, Massachusetts General Hospital; Lead APP, Colorectal Surgery Center and Center for Pelvic Floor Disorders
Daniel Worrall, ANP-BC
Nurse Practitioner, Division of Gastrointestinal and Oncologic Surgery, Massachusetts General Hospital
Ryan Fong, PA-C
OR Robotics, Brigham and Women's Hospital
Nelya Melnitchouk, MD, MSc
Program Director, Colorectal Surgery Fellowship
Director in Peritoneal Surface Malignancy
Brigham and Women's Hospital
Assistant Professor of Surgery, Harvard Medical School
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Describe advances in anal fistula, pilonidal cyst, hemorrhoids, and anal fissure management.
- Identify the current controversies in the management of patients with diverticulitis.
- Review the current treatment pathways and appreciate the nuanced surgical options available to patients with inflammatory bowel disease.
- Describe the importance of having multidisciplinary team input to manage complex pelvic floor conditions.
- Discuss international differences in management of benign colorectal diseases and the importance of international exchange of ideas in surgery.
- Practice new technical skills by participating in hands on workshops on a range of procedures including robotic, laparoscopic, anorectal, and high resolution anoscopy.
[format] => full_html
)
[field_program] => Array
(
[value] => Day 1 - Morning Session 1: International Anorectal Masterclass - Spotlight on Anal Fistula
- What is the ISUCRS and Why Are We Here | Joseph Nunoo-Mensah, MD (Great Britain)
- What Did I Lean on my 4000th Fistula Surgery: Simplified Anogenital Anatomy and Comprehensive Anal Fistula Patterns | Arun Rojanasakul, MD (Thailand)
- Commentary: Lillias Maguire, MD (USA)
- Successful Anal Fistula Surgery Benefits from Preoperative Imaging: A Case for Endoanal Ultrasound | Lucia Oliveira, MD (Brazil)
- Fistulotomy With and Without Immediate Primary Repair | Carlo Ratto, MD (Italy)
- Why We Should Stop Using Setons | Dhatchai Charoensilavath, MD (Thailand)
- Role and Place of VAAFT, FiLAC, Fistura, OTSSC Clip and Fixcision in your Anal Fistula Surgery Arsenal: Serious Procedures or Just Hype? | Joseph Nunoo-Mensah, MD (Great Britain)
- Horseshoe Fistula: Now What? | Ayca Gultekin, MD (Turkey)
- Paul Shellito, MD Lectureship Series: Advanced Anal Fistula Surgery: Partition and Intervention
- Introduction by: Hiroko Kunitake, MD
- Speaker: Arun Rojanasakul, MD (Thailand)
- Commentary: Stanley Goldberg, MD
Day 1 - Morning Session 2: International Pelvic Floor Masterclass: Spotlight on Rectal Prolapse
- Surgery in Patients with Visible External Rectal Prolapse and High-Grade Internal Rectal Intussusception: The European View | Carlo Ratto, MD (Italy)
- Surgery in Patients with Visible External Rectal Prolapse and High-Grade Internal Rectal Intussusception: The UK View | Joseph Nunoo-Mensah, MD (Great Britain)
- Surgery in Patients with Visible External Rectal Prolapse and High-Grade Internal Rectal Intussusception: The USA View | Liliana Bordeianou, MD (USA)
- Recurrent Rectal Prolapse: What Now? | Will Perry, MD (USA)
- Panel Discussion
- Moderator: Liliana Bordeianou, MD
- Panelists: Carlo Ratto, MD (Italy); Liliana Bordeianou, MD (USA); Joseph Nunoo-Mensah, MD (Great Britain); Will Perry, MD (USA); Lieba Savitt, NP; Olga Beresneva, MD; Gonzalo Dhatchai Charoensilavath, MD (Thailand); Gonzalo Hagerman, MD; Margarita Murphy, MD; David Kleiman, MD; Lucia Oliveira, MD; Ayca Gultekin, MD; Rob Goldstone, MD
Day 1 - Morning Session 3: International Anorectal Masterclass: Spotlight on Hemorrhoids, Anal Fissures and Pilonidal Disease
- Anal Fissure: BLINQ, Please | Julia Saraidaridis, MD (USA)
- Hemorrhoids: Anything New To Offer Since WWII | Gonzalo Hagerman, MD (Mexico)
- Complex Pilonidal Diseases: My Favorite Flaps, How I Do Them, and Why | Margarita Murphy, MD (USA)
- Panel Discussion
- Moderator: Grace Lee, MD
- Panelists: Julia Saraidaridis, MD (USA); Gonzalo Hagerman, MD (Mexico); Naomi Goldsmith, MD; Joseph Nunoo-Mensah, MD; Will Perry, MD; Gabriela Möslein, MD; Liliana Bordeianou, MD; Rocco Ricciardi, MD; Lillias Maguire, MD; Thomas Peponis, MD; Carlo Ratto, MD; Holly Bonnette, MD
Day 1 - Afternoon Session 1: The Evolution of Diverticulitis Treatment
- Why Did I Get Diverticulitis and Can I Prevent it From Coming Back? | Julia Saraidaridis, MD (USA)
- Should We Stop Giving Antibiotics to Admitted Patients with Diverticulitis: Lessons from the STAND, AVOD and DIABOLO Trials | Thomas Peponis, MD (USA)
- Setting the Debate Scene: Patient Focused Decision Making in Diverticulitis. How to Decide Who Benefits from an Elective Sigmoid Colectomy? | Jason Hall, MD (USA)
- Arguments for Prompt Surgery: “Enough Already! Just Take The Colon O-U-T OUT!” | Joseph Nunoo- Mensah, MD (Great Britain)
- Arguments for Medical Therapy: “There are Many Effective Strategies to Prevent Recurrent Diverticulitis: First, Do No Harm” | Lillias Maguire, MD (USA)
Day 1 - Afternoon Session 2
- Robotic Sigmoid Resection for Complicated Diverticulitis: Key Technical Points To Master As You Progress On Your Learning Curve | Mark Soliman, MD (USA)
- How Long Can One Sit on a Stable Patient with Perforated Diverticulitis – and Does it Make Sense to Do It? | Thomas Peponis (USA)
- Goodbye, Hartman or Not Quite Yet? | Gabriela Möslein, MD (Germany)
Day 2 - Morning Session 1: Current Surgical Challenges in Inflammatory Bowel Disease Management
- Primer on IBD Meds for the Surgeon: What to Hold and What to Keep Preop and Postop | David Kleiman, MD (USA)
- Surgical Bailouts for a Technically Challenging IPAA: Know Your Options | Jennifer Davids, MD (USA)
- Ernest Codman Lectureship Series: Is Continent Ileostomy In or Out of Fashion Again?
- Introduction by: Christy Cauley, MD
- Speaker: Gabriela Möslein, MD (Germany)
- Segmental or Total Colectomy in UC patients with Dysplasia: Do We Have Any Data for a Rational Decision | Richard Hodin, MD (USA)
- Ileocecal Resection with Various Anastomotic Techniques | Maggie Westfal, MD (USA)
- Does Diversion Have a Place in A Patient with Ileocecal Crohn’s? | Will Perry, MD
- Approaching the Patient with Fistulizing Crohn’s Disease | Joel Goldberg, MD (USA)
Day 2 - Morning Session 2: Complications, Misadventures & Missed Opportunities
- Parastomal Hernia | Rob Goldstone, MD (USA)
- My Colonic Conduit is Dead/Does Not Reach? | Marc Soliman, MD (USA)
- Lower GI Bleeding | Joseph Nunoo-Mensah, MD (Great Britain)
- Stapler Does Not Fit or Pass Through a Kink | Olga Beresneva, MD (USA)
- Anastomotic Leak | Rocco Ricciardi, MD (USA)
- Challenging Stoma | Lucia Oliveira, MD (Brazil)
- Postoperative Ileus | Grace Lee, MD (USA)
- Is Surgery for Slow Transit Constipation Still A Thing? | Kyle Staller, MD (USA)
- Obstetric Anal Sphincter Injury | Carlo Ratto, MD (Italy)
- On Rectovaginal Fistula and Other Surgical Principles Re-Learned During My Missions in Africa | Gonzalo Hagerman, MD (Mexico)
- Is There New Hope for Fecal Incontinence Patients? | Margarita Murphy, MD (USA)
- Panel Discussion
- Moderator: Todd Francone, MD
- Panelists: Rob Goldstone, MD; Marc Soliman, MD (USA); Joseph Nunoo-Mensah, MD (Great Britain); Olga Beresneva, MD (USA); Rocco Ricciardi, MD (USA); Lucia Oliveira, MD (Brazil); Lilian Chen, MD (Germany); Grace Lee, MD (USA); Kyle Staller, MD (USA); Carlo Ratto, MD (Italy); Gonzalo Hagerman, MD (Mexico); Margarita Murphy, MD (USA); Ronald Bleday, MD; Liliana Bordeianou, MD; Christy Cauley, MD; Todd Francone, MD; Joel Goldberg, MD; Grace Lee, MD; Rocco Ricciardi, MD
Day 2 - Afternoon Session: No More Data - Show Us What To Do
Moderator: Rocco Ricciardi, MD
- Anal Fistula: My Favorite Approach | Carlo Ratto, MD (Italy)
- Anal Fistula: My Favorite Approach | Dhatchai Charoensilavath, MD (Thailand)
- Anal Fistula: My Favorite Approach | Joseph Nunoo-Mensah, MD (Great Britain)
- Anal Fistula: My Favorite Approach | Lucia Oliveira, MD (Brazil)
- Pilonidal Cyst: Treatment Depends on Its Grade | Will Perry, MD (USA)
- Pilonidal Cyst: My Favorite Approach | Ayca Gultekin, MD (Turkey)
- Useful Intra- Op Tricks: Using ICG to Your Patient’s Advantage | Olga Beresneva, MD (USA)
- Rectal Prolapse: My Favorite Approach | Liliana Bordeianou, MD (USA)
- Intraoperative Emergency: Stay Calm | Todd Francone, MD (USA)
- Intraoperative Emergency: Stay Calm | Marc Soliman, MD (USA)
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>
This activity is intended for general surgeons, colorectal surgeons, gastroenterologists, urogynecologists, nurse practitioners, physician assistants, nurses, and students.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3828 [id] => 3828 [resource] => accme_data ) [field_show_on_calendar] => [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital, a teaching affiliate of Harvard Medical School in collaboration with the International Society of University Colorectal Surgeons (ISUCRS) and Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=83374
[first] => https://cpd.partners.org/node?nid=83374&page=0
[last] => https://cpd.partners.org/node?nid=83374&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this live activity for a maximum of 4.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 4.5 ANCC contact hour. Nurses should only claim credit commensurate with the extent of their participation in the activity.
Pharmacy
This activity provides 4.5 contact hours (4.5 CEU) of continuing education credit. ACPE Universal Activity Number (UAN): JA0007437-0000-25-003-L99-P
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1739212140
[value2] => 1765601940
[duration] => 26389800
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1762362000
[value2] => 1762380000
[duration] => 18000
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/7
[id] => 7
[resource] => taxonomy_term
[uuid] => 2a38b69f-4c76-44b0-bde5-67e901205c53
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/88302
[id] => 88302
[resource] => file
[uuid] => cf84c987-cf96-4948-b1ff-65f893b99007
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 58868
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Mass General Brigham
[street] => Virtual
[additional] =>
[city] =>
[province] => MA
[postal_code] =>
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => This is a Virtual Course
Climate change and environmental degradation pose serious threats to human health. The primary issue addressed by this course is the significant environmental impact of the United States healthcare system, which contributes substantially to the nation’s greenhouse gas emissions.
This course is designed to foster a more sustainable healthcare system by educating and empowering those in key positions to make impactful changes, as well as those that are curious or committed to becoming more versed in these issues. This course aims to equip clinicians, administrators, and healthcare staff with the knowledge, skills, and resources needed to improve their operations and work towards net zero emissions. By providing education on the environmental impact of healthcare and practical strategies for mitigation, the course empowers participants to implement sustainable practices in their healthcare work environment and through their respective roles.
| Tuition Type | Early Bird (on or before July 31, 2025) | Full Tuition (after July 31, 2025) |
|---|---|---|
| Standard | $145.00 | $175.00 |
| Trainees | $45.00 | $75.00 |
[summary] => [format] => full_html ) [field_course_transcript] => 1 [field_enrollment_requirement_min] => [field_enrollment_requirements] => Array ( ) [field_faculty_credentials] => Array ( [value] =>
Course Directors
 | Wynne Armand, MD |
 | Gregg Furie, MD Medical Director for Climate and Sustainability, Brigham and Women's Hospital |
Faculty
 | Julie Barrios |
 | Latoya P. Brewster, MBA |
 | Jason V. D'Antona |
 | Amanda E. Dilger, MD |
 | Ann-Christine Duhaime, MD |
 | Lucinda L. Everett, MD |
 | Edward Raeke |
 | Jonathan E. Slutzman, MD |
 | Michael Zalis, MD |
[format] => full_html ) [field_hardware_software] => Array ( ) [field_hotel_information] => Array ( ) [field_hotel_link] => Array ( ) [field_hotel_photo] => Array ( ) [field_hotel_travel] => Array ( ) [field_learning_objectives] => Array ( [value] =>
Upon completion of this activity, participants will be able to:
- Recognize the contribution of healthcare in the U.S. to pollution and climate change and the importance of mitigation.
- Quantify the environmental impact of health care.
- Summarize steps for auditing and reporting emissions.
- Discuss non-clinical and clinical pathways to mitigate healthcare greenhouse gas emissions.
- Articulate ways in which participants can work towards net zero emissions.
All presentations will be recorded.
Recordings will be available to all registrants at the conclusion of the live-virtual course.
| 12:00pm | Opening Introduction |
| 12:10 | Healthcare Footprint |
| 12:25 | Measuring Greenhouse Gas Emissions |
| 1:05 | Break |
| 1:15 | Energy |
| 1:55 | Supply Chain |
| 2:35 | Waste |
| 2:55 | Break |
| Clinical Pathways | |
| 3:10 | Evolution of Clinical Decision-Making |
| 3:30 | Breakout Rooms - Choose One
|
| 4:15 | Closing and Q&A |
| 5:00pm | Adjourn |
| Tuition Type | Early Bird (on or before July 31, 2025) | Full Tuition (after July 31, 2025) |
|---|---|---|
| Standard | $145.00 | $175.00 |
| Trainees | $45.00 | $75.00 |
Cancellation Policy:
Registrations cancelled on or before October 22, 2025 will be refunded, less a $20 administrative fee. Registrations cancelled after October 22, 2025 will not be refunded.
Contact mgbcpd@mgb.org if you require assistance in cancelling your online registration.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for health system leaders/administrators and clinicians interested in sustainability careers, including physicians, advanced practice providers, nurses, and pharmacists.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3689 [id] => 3689 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>
Array
(
[self] => https://cpd.partners.org/node?nid=68202
[first] => https://cpd.partners.org/node?nid=68202&page=0
[last] => https://cpd.partners.org/node?nid=68202&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this live activity for a maximum of 1.50 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 1.5 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
Physician Assistants
 Mass General Brigham has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 1.50 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation.
Mass General Brigham has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 1.50 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/231
[id] => 231
[resource] => taxonomy_term
[uuid] => 541dec03-c6af-4bcb-9af7-8fa28fedfb53
)
[1] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/232
[id] => 232
[resource] => taxonomy_term
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1662552000
[value2] => 1685851140
[duration] => 23299140
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1677621600
[value2] => 1683153000
[duration] => 5531400
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/239
[id] => 239
[resource] => taxonomy_term
[uuid] => 8fe8f562-9596-41a9-8e2f-c93aa2c8dae9
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/41510
[id] => 41510
[resource] => file
[uuid] => cdc59ac5-bffd-4758-9a58-2d1662885020
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => Please note, access to symposium recordings is included with registration.
Access will be available for 30 days post event.
With several new drug and cellular therapies as well as an expansion of our understanding of the biologic heterogeneity of hematologic malignancies, there is a need for ongoing education in the area of hematologic malignancies. This interactive webinar series will focus on current best practices and major updates in the biology, diagnosis, and management of hematologic malignancies.
Each 90-minute webinar will have two talks followed by 30 minutes of discussion and audience questions. Presenters will include internationally-known disease experts from Mass General Cancer Center covering practice-changing updates in cellular therapies, transplant, myeloma, leukemia, and lymphoma
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Course Director:
P. Connor Johnson, MD
Hematology/Oncology, Massachusetts General Hospital Cancer Center
Instructor in Medicine, Harvard Medical School
Faculty:
Jeremy Abramson, MD
Director, Jon and Jo Ann Hagler Center for Lymphoma, Massachusetts General Hospital Cancer Center
Associate Professor of Medicine, Harvard Medical School
Andrew Brunner, MD
Assistant Professor of Medicine, Harvard Medical School
Massachusetts General Hospital Cancer Center
Diana Cirstea, MD
Attending Physician
Multiple Myeloma Treatment Program
Massachusetts General Hospital Cancer Center
Zach DeFilipp, MD
Director, BMT Clinical Research, Massachusetts General Hospital Cancer Center
Assistant Professor of Medicine, Harvard Medical School
Areej El-Jawahri, MD
Associate Director, Cancer Outcomes Research and Education Program
Director, Bone Marrow Transplant Survivorship Program, Massachusetts General Hospital Cancer Center
Associate Professor of Medicine, Harvard Medical School
Matt Frigault, MD
Administrative Director, Cellular Therapy Service, Massachusetts General Hospital Cancer Center
Assistant Professor of Medicine, Harvard Medical School
Gaby Hobbs, MD
Clinical Director, Leukemia Service, Massachusetts General Hospital Cancer Center
Assistant in Medicine, Harvard Medical School
Noopur Raje, MD
Director, Center for Multiple Myeloma
Massachusetts General Hospital Cancer Center
Jake Soumerai, MD
Clinical Investigator in Lymphoma, Medicine, Massachusetts General Hospital
Assistant Professor, Medicine, Harvard Medical School
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Identify new therapies available for hematologic malignancies.
- Discuss practice-changing updates in the management of hematologic malignancies.
- Discuss new concepts in palliative care and survivorship.
- Determine appropriate timing to consider transplantevaluation and cellular therapy referral for hematologic malignancies.
[format] => full_html
)
[field_program] => Array
(
[value] => February 28, 2023 - Transplants
Speakers: Zach DeFilipp, MD & Areej El-Jawahri, MD
March 14, 2023 - Leukemia
Speakers: Andrew Brunner, MD & Gaby Hobbs, MD
March 22, 2023 - Cellular Therapies
Speakers: Jeremy Abramson, MD & Matt Frigault, MD
April 12, 2023 - Myeloma
Speakers: Diana Cirstea, MD & Noopur Raje, MD
May 3, 2023 - Lymphoma
Speakers: P. Connor Johnson, MD & Jake Soumerai, MD
[format] => full_html
)
[field_registration_instructions] => Array
(
[value] => CANCELLATION POLICY:
Registrations cancelled on or before February 14, 2023 will be refunded, less a $20 administrative fee. Registrations cancelled after Februrary 14, 2023 will not be refunded.
[summary] =>
[format] => full_html
)
[field_related_courses] => Array
(
)
[field_requirements_max] =>
[field_requirements_min] =>
[field_show_child_catalog] =>
[field_show_child_transcript] =>
[field_target_audience] => Array
(
[value] => This activity is intended for physicians, nurses, physician assistants, other members of healthcare team (regional) with specialties such as general practice, hematology, hematology/oncology, medical oncology, primary care, and radiation oncology.
[format] => full_html
)
[field_venue_phone] => Array
(
)
[upload] => Array
(
)
[field_accme_data] => Array
(
[uri] => https://cpd.partners.org/accme_data/3051
[id] => 3051
[resource] => accme_data
)
[field_show_on_calendar] =>
[field_custom_provided] => Array
(
[value] => Massachusetts General Hospital Cancer Center & Mass General Brigham
[summary] =>
[format] => full_html
)
[field_course_exhibitor] => Array
(
)
[field_course_qualifiers] => Array
(
)
[field_course_image_cards] => Array
(
)
[field_income_expense] => Array
(
)
[og_membership] => Array
(
)
[og_membership__1] => Array
(
)
[og_membership__2] => Array
(
)
[og_membership__3] => Array
(
)
[og_group_ref__og_membership] => Array
(
)
[og_group_ref__og_membership__1] => Array
(
)
[og_group_ref__og_membership__2] => Array
(
)
[og_group_ref__og_membership__3] => Array
(
)
[flag_course_bookmark_user] => Array
(
)
[model] => course_68202
[list_price] => 0.00000
[cost] => 0.00000
[sell_price] => 149.00000
[price] => 149.00000
[weight] => 0
[weight_units] => lb
[length] => 0
[width] => 0
[height] => 0
[length_units] => in
[pkg_qty] => 1
[ordering] => 0
[shippable] => 0
[nid] => 68202
[vid] => 182197
[is_new] =>
[type] => course
[title] => Hematologic Malignancies 2023-DO NOT USE
[language] => und
[url] => https://cpd.partners.org/content/hematologic-malignancies-2023-do-not-use
[edit_url] => https://cpd.partners.org/node/68202/edit
[status] => 1
[promote] => 1
[sticky] => 1
[created] => 1699451200
[changed] => 1705430544
[author] => Array
(
[uri] => https://cpd.partners.org/user/92
[id] => 92
[resource] => user
[uuid] => 48adffb8-b573-4cd5-ada8-52d9bb7f0770
)
[log] =>
[revision] =>
[course] => Array
(
[uri] => https://cpd.partners.org/course/68202
[id] => 68202
[resource] => course
)
[book_ancestors] => Array
(
)
[comment] => 1
[comments] => Array
(
)
[comment_count] => 0
[comment_count_new] => 0
[body] => Array
(
)
[feeds_item_guid] =>
[feeds_item_url] =>
[feed_nid] =>
[relation_faculty_user] => Array
(
)
[uuid] => 4888bd1f-1ff5-40fd-b3d2-a423dfe74aa2
[vuuid] => 9bc55e94-62dc-4433-85dd-233037ca3b2d
)
)
)
Array
(
[self] => https://cpd.partners.org/node?nid=52303
[first] => https://cpd.partners.org/node?nid=52303&page=0
[last] => https://cpd.partners.org/node?nid=52303&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => Accreditation (per session):
In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditTM
Mass General Brigham designates this live activity for a maximum of 1 AMA PRA Category 1 CreditTM . Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 1 ANCC contact hour. Nurses should only claim credit commensurate with the extent of their participation in the activity.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/233
[id] => 233
[resource] => taxonomy_term
[uuid] => 6eaae05a-320b-4526-8ffd-84176655943f
)
[1] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/229
[id] => 229
[resource] => taxonomy_term
[uuid] => a9f7b985-9122-42ff-ab40-57b988c61135
)
[2] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/230
[id] => 230
[resource] => taxonomy_term
[uuid] => 32cd4c1a-e494-4fb3-9e83-4edb7b43c8e2
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1662048000
[value2] => 1674684000
[duration] => 12636000
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/238
[id] => 238
[resource] => taxonomy_term
[uuid] => fd81c17a-d19b-46b8-ad6b-2c5aee9ce9be
)
[1] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/239
[id] => 239
[resource] => taxonomy_term
[uuid] => 8fe8f562-9596-41a9-8e2f-c93aa2c8dae9
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/41567
[id] => 41567
[resource] => file
[uuid] => bf41775a-5e95-450e-83c7-a733871dae21
)
)
[field_course_intro] => Array
(
)
[field_course_live] =>
[field_course_location] => Array
(
[lid] => 28986
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Massachusetts General Hospital
[street] =>
[additional] =>
[city] => Boston
[province] => MA
[postal_code] => 02114
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => Description
Value-based health care focuses on improving patient health outcomes while reducing health care costs over time. Value-based care benefits all stakeholders in health care: first and foremost, patients, but also providers, healthcare systems, payors, and society at large. However, achieving value-based health outcomes for patients remain low and stagnating at unacceptable levels and all stakeholders remain frustrated.
This lecture series presented by the Massachusetts General Hospital, Department of Neurology’s Center for Value-Based Health Care and Science will inform how well-established frameworks (implementation science and quality improvement) can address unsolved healthcare problems. Additionally, it will serve as a first step for health care providers to learn about these methods and how they can help improve their practice. As a desired result of this educational activity, providers and teams will be able to design and implement value-based healthcare projects and enhance patient reported outcomes across multiple conditions and care settings.
This course consists of 10 weekly lectures from October 2022 to January 2023. Seminars will feature lectures and interactive activities lead by experts with extensive experience in value-based health care and/or sciences. These leaders in the field will share what they have learned and their own methods for overcoming barriers in traditional health care systems to develop successful health care delivery models. Special emphasis will be places on utilizing these methods to tackle and prevent health inequities.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Lidia Moura, MD, PhD, MPH - Course Director
Associate Professor of Neurology,
Harvard Medical School;
Co-director, Center for Value-based Health Care and Sciences,
Principal Investigator, NeuroValue Laboratory,
Massachusetts General Hospital;
Chief Health Informatics Officer,
Epilepsy Foundation of America
Sahar Zafar, MD, MSc - Course Director
Assistant Professor of Neurology,
Harvard Medical School;
Co-director, Center for Value-based Health Care and Sciences,
Associate Medical Director, MGH Neuroscience Intensive Care Unit,
Massachusetts General Hospital;
Director, Mass General Brigham Neurocritical Care Fellowship,
Mass General Brigham
Amanda Guidon, MD, MPH - Course Director
Assistant Professor of Neurology,
Harvard Medical School;
Education & Dissemination Lead, Center for Value-based Health Care and Sciences,
Director, Myasthenia Gravis Clinic, MGH,
Massachusetts General Hospital;
Director, Neuromuscular Medicine Fellowship,
Mass General Brigham
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Define important value-based healthcare and/or sciences terminology.
- Contrast the differences, similarities, and applications of quality improvement and implementation frameworks in healthcare.
- Recognize how each participant’s unique role in their teams can utilize quality improvement methods and techniques.
- Extrapolate implementation, change management, and quality improvement methods to participants’ own practices and as it relates to their role in their teams
- Construct and organize a value-based healthcare and/or research team
- Reflect and study value-based initiatives and use those insights to plan future advancements
- Identify how to use value-based health care methods to address health inequalities related to:
- Telemedicine
- Racial, Ethnic, and Language Minority patient populations
- Sexual and Gender Minority patient populations
- Clinical Research Trials
[format] => full_html
)
[field_program] => Array
(
[value] => Part A: Introduction to Value-Based Science Concepts and Methods
Parts A and B will overview what value-based science methods are, the use of different frameworks and methods in healthcare.
October 31, 2022 | Lecture 1: |
|
November 9, 2022 | Lecture 2: |
|
November 16, 2022
| Lecture 3: |
|
Part B: Applying Value-Based Science (Concept to Reality)
November 30, 2022 | Lecture 4: |
|
December 7, 2022 | Lecture 5: |
|
December 13, 2022 | Lecture 6: |
|
Part C: Using Value-based Methods to Address Health Inequities
A special focus will be placed in this program on methods to assess and address care disparities.
January 4, 2023 | Lecture 7: |
|
January 11, 2023 | Lecture 8: |
|
January 18, 2023 | Lecture 9: |
|
January 25, 2023 | Lecture 10: |
|
This activity is intended for healthcare professionals and staff including providers (faculty, residents, fellows, and advanced practice providers), nurses, and research staff with involvement or interest in improving health care systems.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/2315 [id] => 2315 [resource] => accme_data ) [field_show_on_calendar] => [field_custom_provided] => Array ( [value] =>Center for Value-Based Health Care and Sciences, Department of Neurology, Massachusetts General Hospital and Mass General Brigham
![]()
Array
(
[self] => https://cpd.partners.org/node?nid=84311
[first] => https://cpd.partners.org/node?nid=84311&page=0
[last] => https://cpd.partners.org/node?nid=84311&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => This activity is not for credit.
The recording is being offered as a resource for those who did not register for the live conference on April 11, 2025.
[summary] =>
[format] => full_html
)
[field_course_catalog] =>
[field_course_category] => Array
(
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1744812000
[value2] => 1776311940
[duration] => 31499940
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/80725
[id] => 80725
[resource] => file
[uuid] => e897be3b-dc3a-411f-a26b-72fe3b277d02
)
)
[field_course_intro] => Array
(
)
[field_course_live] =>
[field_course_location] => Array
(
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => This is a recording of the April 11th conference.
The second Community Care in Reach® (CCiR) Mobilizing Addiction Services conference will highlight strategies & best practices around mobilizing clinical care and harm reduction services for people living with addiction. Subject matter experts from across the country will present their expertise & knowledge on topics spanning several aspects of mobile and addiction care, including safety & de-escalation in a mobile setting, the role of mobile programs in combatting stigma around addiction, and how to navigate providing addiction care in our evolving political and social landscape.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] =>  | Elsie Taveras, MD, MPH - Course Director Chief Community Health & Equity Officer, Mass General Brigham Executive Director, Kraft Center for Community Health at Massachusetts General Hospital Conrad Taff Professor of Pediatrics in Nutrition, Harvard Medical School Professor in the Department of Nutrition, Harvard T.H. Chan School of Public Health |
 | Erik Garcia, MD Erik Garcia, MD has been been providing healthcare to adults experiencing homelessness for the entirety of his career – starting when he completed his Internal Medicine residency in 1994. He is married to a doctor (the research, PhD kind…"smarter than me" he says) who is incredibly supportive. They have 2 grown kids who (while they have avoided the medical field) have a wonderful sense of social consciousness. |
 | Sarah Mackin, MPH Sarah Mackin, MPH is the director of AHOPE Needle Exchange at the Boston Public Health Commission, where she began her work in harm reduction and drug user health in 2010. She oversees the largest needle exchange and harm reduction program in New England, which provides comprehensive drug user health services to over 8,000 people each year. Sarah brings over 18 years of experience in the field of public health, substance use, harm reduction, HIV/AIDS, and homelessness to the work. |
 | Maritza Perez Medina, JD Maritza Perez Medina manages DPA's federal legislative agenda and advocacy strategy in Congress as well as DPA’s general engagement with the federal government on its policy priorities. Previously, Maritza was a Senior Policy Analyst for Criminal Justice Reform at the Center for American Progress (CAP). Prior to joining CAP, Maritza was a Legislative Staff Attorney at the Mexican American Legal Defense and Educational Fund (MALDEF) where she advocated on a range of civil rights issues impacting Latino communities. Originally from Nevada, Maritza obtained her B.A. from the University of Nevada, Reno with academic honors, graduating with double majors in journalism and Spanish and double minors in political science and economic policy. She earned her J.D. at the University of California, Berkeley, School of Law, receiving the highest distinction upon graduation for her pro bono work, and is licensed to practice law in the District of Columbia and in the state of California. A criminal justice and drug policy expert, Maritza has been featured in various media outlets including The Washington Post, The New York Times, Los Angeles Times, The Wall Street Journal, Politico, Roll Call, The Boston Globe, CNN, USA Today, Chicago Tribune, NPR, Latino USA, and more. |
 | Kenneth Washington Kenneth Washington is an accomplished assistant director of AHOPE Needle Exchange, driven by a passion for harm reduction that stems from his work with at-risk youth. His lived experience has instilled in him a deep understanding of the challenges of racism, classism, and substance use, inspiring him to become a leader in the field. Kenneth's outstanding achievements in harm reduction have earned him a seat on the Massachusetts Harm Reduction Advisory Council, a testament to his unwavering dedication to public service. His desire to help his community has led him to excel in drug checking and introduce innovative safer smoking practices to the Boston area outreach. With his profound knowledge and expertise, Kenneth has made a significant impact on the lives of countless individuals and helped to shape policies that promote safer and healthier communities. His contributions have been widely recognized and admired by peers, colleagues, and stakeholders alike. |
Since the content of this activity is non-clinical, disclosure forms do not need to be collected for planners and speakers.
[format] => full_html ) [field_hardware_software] => Array ( ) [field_hotel_information] => Array ( ) [field_hotel_link] => Array ( ) [field_hotel_photo] => Array ( ) [field_hotel_travel] => Array ( ) [field_learning_objectives] => Array ( [value] =>Upon completion of this activity, participants will be able to:
- Describe the CCiR mobile addiction services model that uses cross-sector collaborations to reduce siloing of services, especially between harm reduction and clinical care.
- Apply safety and de-escalation strategies for teams on mobile units.
- Apply effective strategies for destigmatizing addiction care in mobile settings.
- Assess elements of effective outreach and engagement.
- Design an effective community engagement strategy in advance of mobile program launch.
- Describe local, regional, and national trends, events, and contexts that may impact a mobile team’s ability to provide effective addiction and harm reduction services.
- Use strategies to effectively provide and advocate for mobile addiction care considering new developments in the legal, political, and social landscape.
| Time Stamp | Lecture Title & Speaker |
| 00:00:14 | Introduction & Welcome Elsie Taveras, MD, MPH |
| 00:07:31 | Combating Addiction Stigma: What Role Can Mobile Programs Play? Erik Garcia, MD |
| 1:19:00 | De-Escalation & Staying Safe in Close Quarters Sarah Mackin, MPH & Kenneth Washington |
| 2:24:00 | Changing Political Climate: Tools & Resources Maritza Perez Medina, JD |
| 3:20:00 | Closing Remarks Julie Burns |
This activity is intended for physicians, nurses, social workers and other members of the healthcare team with specialties of addiction medicine & primary care.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3768 [id] => 3768 [resource] => accme_data ) [field_show_on_calendar] => [field_custom_provided] => Array ( [value] =>Kraft Center for Community Health, Massachusetts General Brigham Center for Community Health, RIZE Massachusetts & Mass General Brigham


Array
(
[self] => https://cpd.partners.org/node?nid=83166
[first] => https://cpd.partners.org/node?nid=83166&page=0
[last] => https://cpd.partners.org/node?nid=83166&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Mass General Brigham designates this live activity for a maximum of 5.50 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Lifelong Learning Maintenance of Certification (MOC) Program
MOC RECOGNITION STATEMENT
Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to 5.50 MOC points in the American Board of Internal Medicine’s (ABIM) Maintenance of Certification (MOC) program. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/244
[id] => 244
[resource] => taxonomy_term
[uuid] => 41b0f6bc-954e-439d-b355-009eb871e393
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1737988740
[value2] => 1744171140
[duration] => 6182400
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1741437900
[value2] => 1741460400
[duration] => 22500
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/81717
[id] => 81717
[resource] => file
[uuid] => e1bdf03a-d607-423d-8b1c-2951cff8fbdb
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => This is a virtual course
This webinar is focused on raising awareness about colorectal cancer in Africa. Colorectal cancer is preventable with screening & surveillance tools, and most high-income countries have well-established prevention and early detection programs. However, most African countries lack structured colorectal cancer screening protocols & guidelines, resulting in incomplete epidemiologic data and many preventable cancer cases & deaths.
This symposium will focus on understanding the magnitude of colorectal cancer epidemiology & risk factors in Africa, and on opportunities for improved screening programs. In addition, speakers will present a multidisciplinary approach to management of colorectal cancer, including initial diagnosis, staging & treatment options (e.g. medical management, surgical intervention & palliative care). The symposium will also serve as an opportunity to develop collaborations & networking amongst participants involved in the care of African patients with colorectal cancer.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Course Co-Directors
Akwi W. Asombang, MD, MPH
Interventional Gastroenterologist, Massachusetts General Hospital
Director of Global Health Programs for Gastroenterology, Massachusetts General Hospital
Co-Founder, Pan-African Organization for Health Education & Research (POHER)
Founder, The African Association of Future Gastroenterologists (AAFG)
Segun Komolafe, MD
General & Colorectal Surgeon, University Hospital Wishaw
Clinical Lead for Colorectal Cancer, NHS Lanarkshire, United Kingdom
Mukhtar Ahmad, MD
Consultant Colorectal Surgeon and Lead Clinician for Colorectal Surgery, University Hospitals Dorset, United Kingdom
Faculty
Cesare Hassan, MD
Rich Harlan, MD
Chinenye Iwuji, MD
Amina Kidee, MD
Dickson Mupeta
Chidi Nnabuchi, MD
Christian Ntizimira, MD
Andrew Odhiambo, MD
Ganiyat Oyeleke, MD
Olorunda Rotimi, MD
Abbas Rupawala, MD
Manoj Thillai, MD
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Discuss the trends of colorectal cancer in Africa
- Summarize updates of colorectal cancer screening & Surveillance in Africa
- Describe the role of multidisciplinary team approach to management of colorectal cancer
- Describe local & global approaches to bowel preparation in the context of colorectal cancer screening
- Discuss medical & surgical management of colorectal cancer
- Discuss the role of palliative care in the management of colorectal cancer
- Develop & establish colorectal cancer screening programs
[format] => full_html
)
[field_program] => Array
(
[value] => | 7:50 AM | Welcome & Introduction | Akwi W. Asombang, MD, MPH |
| SESSION 1 | Moderator: Ganiyat Oyeleke, MD | |
| 8:00 | Epidemiology of Colorectal Cancer in Africa | Chidi Nnabuchi, MD |
| 8:25 | Bowel Preparation Options | Rich Harlan, MD |
| 8:50 | How to Establish a Colorectal Cancer Screening Program | Cesare Hassan, MD |
| 9:10 | Q & A |
| 9:20 | Break |
| SESSION 2 | Moderator: Segun Komolafe, MD | |
| 9:30 | Risk Factors & Medical Management of Early Onset Colorectal Cancer | Amina Kidee, MD |
| 9:55 | Surgical Management of Colon vs. Rectal Cancer | Mukhtar Ahmad, MD |
| 10:20 | IBD and CRC: When to Screen & How? | Abbas Rupawala, MD |
| 10:40 | Q & A |
| 10:50 | Break |
| SESSION 3 | Moderator: Mukhtar Ahmad, MD | |
| 11:00 | Pathology of IBD Related CRC | Olorunda Rotimi, MD |
| 11:25 | Challenges in Management of CRC in Resource Limited Settings | Chinenye Iwuji, MD |
| 11:50 | Liver Transplantation in patients with Metastatic CRC | Manoj Thillai, MD |
| 12:10 PM | Q & A |
| 12:20 | Break |
| SESSION 4 | Moderators: Chidi Nnabuchi, MD & Mr. Dickson Mupeta | |
| 12:30 | Palliative Care in Colorectal Cancer | Christian Ntizimira, MD |
| 12:55 | Patient Advocacy: Personal Story | Andrew Odhiambo, MD |
| 1:15 | Q & A |
| 1:30 | Wrap Up & Discussion of Next Steps | Akwi W. Asombang, MD, MPH, Segun Komolafe, MD, Mukhtar Ahmad, MD, Ganiyat Oyeleke, MD & Chidi Nnabuchi, MD |
| 2:00 PM | Adjournment |
[format] => full_html ) [field_registration_instructions] => Array ( [value] =>
| Registration Type | Tuition Fee |
|---|---|
| US-Based Healthcare Professionals | $50 |
| Non-US Based Healthcare Professionals (CE Credit) | $50 |
| Non-US Based Healthcare Professions (No CE Credit) | Free |
This activity is intended for physicians, nurses & other members of the healthcare system.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3683 [id] => 3683 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital & Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=77145
[first] => https://cpd.partners.org/node?nid=77145&page=0
[last] => https://cpd.partners.org/node?nid=77145&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => Accreditation
In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditTM
Mass General Brigham designates this live activity for a maximum of 1 AMA PRA Category 1 CreditTM. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 1 ANCC contact hour. Nurses should only claim credit commensurate with the extent of their participation in the activity.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1724083200
[value2] => 1747933200
[duration] => 23850000
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/238
[id] => 238
[resource] => taxonomy_term
[uuid] => fd81c17a-d19b-46b8-ad6b-2c5aee9ce9be
)
[1] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/237
[id] => 237
[resource] => taxonomy_term
[uuid] => 842d3b08-d27d-4a11-8281-71bcfb00ec51
)
[2] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/239
[id] => 239
[resource] => taxonomy_term
[uuid] => 8fe8f562-9596-41a9-8e2f-c93aa2c8dae9
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/54406
[id] => 54406
[resource] => file
[uuid] => 71939cdf-376f-4fbf-9bc0-e93579d78d2b
)
)
[field_course_intro] => Array
(
)
[field_course_live] =>
[field_course_location] => Array
(
[lid] => 45473
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Massachusetts General Hospital
[street] =>
[additional] =>
[city] => Boston
[province] => MA
[postal_code] => 02114
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => Massachusetts General Hospital
Cancer Center Grand Rounds 2024-2025
September 19, 2024 - May 22, 2025
Back again the 2024-2025 Cancer Center Grand Rounds are available to the public to attend virtually LIVE via paid subscription.
(Please note: This subscription does not include in-person attendance)
The theme of the series is "Early Detection" and kicks off Thursday September 19, 2024 at 12:00 PM EDT. The series will cover a comprehensive array of disease areas and topics, attendees will be provided with a robust selection of sessions to bring them up to speed on the most cutting-edge research and therapies in oncology.
The subscription will provide access to BOTH the live webinar AND the recording; however, if claiming credit, you may only claim credit for attending one or the other per date.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Colin D. Weekes, MD, PhD - Course Director
Director, Medical Oncology Research for Pancreatic Cancer,
Director, Cancer Center Grand Rounds Program
Massachusetts General Hospital
Douglas Micalizzi, MD, PhD
Clinical Director, Cancer Early Detection and Diagnostics Clinic,
Massachusetts General Hospital Cancer Center
Lecia Sequist, MD, MPH
Program Director, Cancer Early Detection and Diagnostics Clinic,
Massachusetts General Hospital Cancer Center;
Landry Family Professor of Medicine
Harvard Medical School
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
[value] => Participation is online streaming – broadcast from Massachusetts General Hospital.
After you register, you will receive an email with details for how to participate.
[format] => full_html
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Evaluate recent advances in early detection research and programs presented in this series
- Assess opportunities to integrate early detection into how you support research
- Assess opportunities to integrate early detection practices & strategies into how you deliver patient care
- Recognize the impact and evolving landscape of early detection in cancer care worldwide
[format] => full_html
)
[field_program] => Array
(
[value] => Sessions will be held weekly on Thursday from September 19, 2024 to May 22, 2025 from 12:00 to 1:00 PM.
| Date | Subject | Speaker |
|---|---|---|
September 19, 2024 | Why Should Cancer Centers Develop a Focus on Early Detection? | Moderator: Panelists: Douglas Micalizzi, MD, PhD Erica Warner, ScD Elsie Taveras, MD, MP |
September 26, 2024 | Infectious Disease MGH, A Global View on Virally-Mediated Cancer Risk, Cervical Cancer | Ruanne Barnabas, MBChB, MSc, DPhil |
October 10, 2024 | “How I Live” Cancer Documentary – Storytelling Strategies to Impact Change | Irini Ablanti, DrPH, MPH, MA Meghan Shea Soad Fuentes- Alabí, MD, MPH Flo Awde, MAS |
October 31, 2024 | The Grand Challenge of Cancer Disparities | Melissa Davis, PhD |
November 7, 2024 | “Space-Based Research- Predicting and Preventing Accelerated Stem Cell Aging & Cancer Evolution | Catriona Jamieson, MD, PhD |
November 14, 2024 | Multi-Cancer Detection Assays: Hope or Hype? | Moderator: Panelists: Gil Welch, MD Betsy O’Donnell, MD |
December 5, 2024 | Early detection of high grade serous endometrial and ovarian cancers. One step ahead. | Lucy Gilbert, MD, MSc, FRCOG |
December 19, 2024 | Lung Cancer Screening as an Opportunity for Community Outreach and Engagement | Moderator: Panelists: Rian Hasson, MD, MPH, FACS Michael Gieske, MD |
January 9, 2025 | Ash Update | Michelle Lee, MD Ben Puliafito, MD Jeremy Abramson, MD Richard Newcomb, MD Debbie Jiang, MD |
January 16, 2025 | Germline Predisposition to Hematopoietic Malignancies | Lucy Godley |
January 23, 2025 | Junior Scientist Lectures | Avinash Mishra |
January 30, 2025 | Military Service as a Risk Factor for Cancer and What We Can Do About It | Moderator: Panelists Allison Jaslow Paul Martin |
February 13, 2025 | Engineering Imaging Tools to Improve Early Cancer Detection and Prevention | Rebecca Richards-Kortum, PhD |
February 27, 2025 | Early Detection of MRD: A Path Towards Curing More Patients with CRC | Aparna Parikh, MD |
March 6, 2025 | Myeloma: Pillars of Progress | Sagar Lonial, MD, FACP |
| March 13, 2025 | Thinking about Germline Risk in 2024 | Moderator: Panelists: Susan Domchek, MD Matthew Yurgelun |
March 20, 2025 | How Can AI Help Intercept Cancer? | Moderator: Panelists: Chris Sander, PhD Eleni Linos, MD, MPH, DPhil Keyan Salari, MD, PhD |
March 27, 2025 | TBD | Shawn Demehri, MD, PhD |
April 3, 2025 | The Chabner Pioneers in Oncology Lectureship: How Altered Metabolism Influences Cancer Progression | Matthew G. Vander Heiden |
April 10, 2025 | Is it Time to Rethink PSA Screening? | Moderator: Panelists: Brandon Mahal Michael Barry |
April 17, 2025 | The Promise of Goal Concordant Care: Can We Deliver? | Timothy Pawlick |
May 1, 2025 | ACS-IRG Scholars | Patrick Connor Johnson, MD Catherine Meador, MD, PhD Peter Miller, MD, PhD Uma Sachdeva, MD, PhD Jaime Schneider, MD, PhD |
May 15, 2025 | State of Cancer | Robert Smith, PhD |
| Registration Type | Tuition Price |
|---|---|
| All Registrants | $50.00 |
For questions regarding the registration process, please contact Mass General Brigham Office of Continuing Professional Development at mgbcpd@mgb.org.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for research and clinical staff who need to be educated on cutting edge information on advances and perspectives on cancer research and treatment across the full spectrum of cancer specialization.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3387 [id] => 3387 [resource] => accme_data ) [field_show_on_calendar] => [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital Cancer Center and Mass General Brigham
[summary] => [format] => full_html ) [field_course_exhibitor] => Array ( ) [field_course_qualifiers] => Array ( ) [field_course_image_cards] => Array ( ) [field_income_expense] => Array ( ) [og_membership] => Array ( ) [og_membership__1] => Array ( ) [og_membership__2] => Array ( ) [og_membership__3] => Array ( ) [og_group_ref__og_membership] => Array ( ) [og_group_ref__og_membership__1] => Array ( ) [og_group_ref__og_membership__2] => Array ( ) [og_group_ref__og_membership__3] => Array ( ) [flag_course_bookmark_user] => Array ( [0] => Array ( [uri] => https://cpd.partners.org/user/12500 [id] => 12500 [resource] => user [uuid] => de36a2e6-c45a-49cf-9c20-d4adfc342336 ) [1] => Array ( [uri] => https://cpd.partners.org/user/13623 [id] => 13623 [resource] => user [uuid] => 99174dc0-ee8c-4afb-9a25-a8f8e52f9193 ) [2] => Array ( [uri] => https://cpd.partners.org/user/132374 [id] => 132374 [resource] => user [uuid] => d2aac272-e155-4cf5-bad4-feb4d25b84d0 ) ) [model] => course_77145 [list_price] => 0.00000 [cost] => 0.00000 [sell_price] => 50.00000 [price] => 50.00000 [weight] => 0 [weight_units] => lb [length] => 0 [width] => 0 [height] => 0 [length_units] => in [pkg_qty] => 1 [ordering] => 0 [shippable] => 0 [nid] => 77145 [vid] => 227568 [is_new] => [type] => course [title] => MGH Cancer Center Grand Rounds 2024-2025 - Subscription [language] => und [url] => https://cpd.partners.org/content/mgh-cancer-center-grand-rounds-2024-2025-subscription [edit_url] => https://cpd.partners.org/node/77145/edit [status] => 1 [promote] => 0 [sticky] => 0 [created] => 1724346607 [changed] => 1744754636 [author] => Array ( [uri] => https://cpd.partners.org/user/257 [id] => 257 [resource] => user [uuid] => bd6fd397-09cf-4275-a7d4-35783f50f323 ) [log] => [revision] => [course] => Array ( [uri] => https://cpd.partners.org/course/77145 [id] => 77145 [resource] => course ) [book_ancestors] => Array ( ) [comment] => 1 [comments] => Array ( ) [comment_count] => 0 [comment_count_new] => 0 [body] => Array ( ) [feeds_item_guid] => [feeds_item_url] => [feed_nid] => [relation_faculty_user] => Array ( ) [uuid] => 668ebd23-9034-482d-9156-90c39edbd925 [vuuid] => 3737a141-6173-4762-ab20-a376b26f8975 ) ) )Array
(
[self] => https://cpd.partners.org/node?nid=59175
[first] => https://cpd.partners.org/node?nid=59175&page=0
[last] => https://cpd.partners.org/node?nid=59175&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => enrolled
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 Credits™
Mass General Brigham designates this live activity for a maximum of 5.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 5.5 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
Physician Assistants
Mass General Brigham has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for 5.5 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation.

Pharmacy
This activity provides 5.5 contact hours (5.5 CEUs) of continuing education credit. ACPE Universal Activity Number (UAN): JA0007437-0000-24-009-L99-P
MOC Recognition Statement
Successful completion of this CME activity, which includes participation in the activity, with individual assessments of the participant and feedback to the participant, enables the participant to earn 5.5 MOC points in the American Board of Internal Medicine (ABIM) Maintenance of Certification (MOC) program. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/197
[id] => 197
[resource] => taxonomy_term
[uuid] => 621a8034-627c-4c33-b273-260b2d83768c
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1687868220
[value2] => 1716609540
[duration] => 28741320
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1709904600
[value2] => 1709928900
[duration] => 24300
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/7
[id] => 7
[resource] => taxonomy_term
[uuid] => 2a38b69f-4c76-44b0-bde5-67e901205c53
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/51758
[id] => 51758
[resource] => file
[uuid] => 459a5606-52b5-4359-83c6-d40a100b6d18
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 44311
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Livestream
[street] => Massachusetts General Hospital
[additional] =>
[city] => Boston
[province] => MA
[postal_code] => 02114
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => This is a virtual course
The MGH Pericardial Disease Symposium will be a one-day live virtual course dedicated to providing a contemporary overview of common pericardial diseases, specifically highlighting the presentation, diagnosis, and management of acute pericarditis, recurrent pericarditis, and constrictive pericarditis. The course will feature evidence-based educational strategies including case presentations, didactic lectures, patient perspectives, and complex case round-table discussions to foster an interactive, collaborative, and multi-disciplinary learning environment.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Course Directors
Jonathan Salik, MD, MS
Assistant Inpatient Education Director, Cardiology Division,
Associate Program Director for Elective and Subspecialty Training, Internal Medicine Residency Program,
Massachusetts General Hospital;
Instructor, Harvard Medical School
Thoralf Sundt, MD

Chief, Division of Cardiac Surgery, Co-Director of the Corrigan Minehan Heart Center, Massachusetts General Hospital;
Professor of Surgery, Harvard Medical School
Shana Osho, MD, MPH

Cardiac Surgeon, Massachusetts General Hospital;
Assistant Professor of Surgery, Harvard Medical School
Faculty
George Blees
Patient
Jonathan Hausmann, MD
Rheumatologist, Boston Children's Hospital and Massachusetts General Hospital;
Assistant Professor of Medicine, Harvard Medical School
Emily Lau, MD, MPH
Instructor in Medicine, Harvard Medical School;
Director, Hormones & Cardiovascular Disease Clinic, Massachusetts General Hospital
Leonard Lilly, MD
Cardiology Section Chief, Brigham and Women's Hospital;
Professor, Harvard Medical School
Tomas Neilan, MD, MPH
Director, Cardio-Oncology Program,
Co-Director, Cardiac MR PET CT Program, Massachusetts General Hospital;
Associate Professor of Medicine, Harvard Medical School
Michael Picard, MD
Cardiologist, Massachusetts General Hospital;
Professor, Harvard Medical School
Baileigh Rolfe
Patient
Ada Stefanescu, MD
Interventional Cardiologist, Massachusetts General Hospital;
Instructor in Medicine, Harvard Medical School
Albree Tower-Rader, MD
Cardiologist, Massachusetts General Hospital;
Instructor of Medicine, Harvard Medical School
Brittany Weber, MD, PhD
Director of Cardio-Rheumatology Clinic, Brigham and Women's Hospital;
Instructor of Medicine, Harvard Medical School
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Session 1: Acute Pericarditis:
Upon completion of this activity, participants will be able to:
- Identify optimal treatment strategies for acute pericarditis.
- Compare different approaches to pericardiocentesis and identify benefits/limitations to each approach.
- Recognize signs of connective tissue disease in patients with acute pericarditis and identify common rheumatologic conditions associated with acute pericarditis.
Session 2: Recurrent Pericarditis:
Upon completion of this activity, participants will be able to:
- Identify hallmark features of recurrent and constrictive pericarditis on advanced cardiac imaging.
- Describe the mechanisms of auto-inflammation associated with recurrent pericarditis and identify novel treatment strategies that intercede on these pathways.
- Summarize the treatment algorithm for recurrent pericarditis and identify emerging indications for the use of IL-1 inhibitors.
Session 3: Constrictive Pericarditis:
Upon completion of this activity, participants will be able to:
- Describe the pathophysiology and hemodynamics of constrictive pericarditis.
- Recognize echocardiographic manifestations of constrictive pericarditis.
- Identify indications for pericardiectomy and compare approaches to surgical treatment
Social Media
Twitter:
Mass General Brigham Professional Development
@MassGenBrighCPD
MGH Corrigan Minehan Heart Center
@MGHHeartHealth
LinkedIn:
Mass General Brigham Professional Development
FUNDING
Pericardial Disease Symposium has received support in the form of an educational grant from the following companies:
Cardiol Therapeutics Inc.
Kiniksa Pharmaceuticals, Ltd.
[format] => full_html
)
[field_program] => Array
(
[value] => Session 1: Acute Pericarditis: The Basics | |
| 8:30am | Welcome and Overview | Jonathan Salik, MD, MS |
| 8:35 | Case Presentation | Fellow |
| 8:40 | Diagnosis and Treatment of Acute Pericarditis | Emily Lau, MD, MPH |
| 8:55 | Pericardiocentesis: What Every Clinician Should Know | Ada Stefanescu, MD |
| 9:10 | Pericarditis in Systemic Disease | Jonathan Hausmann, MD |
| 9:25 | Q&A | Jonathan Salik, MD, MS; Ada Stefanescu, MD; Jonathan Hausmann, MD |
| 9:40 | Complex Case Round Table | Jonathan Salik, MD, MS; Ada Stefanescu, MD; Jonathan Hausmann, MD |
| 10:00 | BREAK |
Session 2: Recurrent Pericarditis: A Vexing Challenge | |
| 10:15 | Case Presentation | Fellow |
| 10:20 | Making the Diagnosis: Advanced Imaging Techniques for Pericardial Disease | Albree Tower-Rader, MD |
| 10:40 | Approach to the Treatment of Recurrent Pericarditis | Jonathan Salik, MD, MS |
| 10:55 | Autoinflammation, IL-1 Inhibitors, and Novel Therapies | Brittany Weber, MD, PhD |
| 11:15 | Q&A | Albree Tower-Rader, MD; Jonathan Salik, MD, MS; Brittany Weber, MD, PhD |
| 11:30 | Recurrent Pericarditis: The Patient Perspective | Baileigh Rolfe & Jonathan Salik, MD, MS |
| 11:40 | Complex Case Round Table | Albree Tower-Rader, MD; Jonathan Salik, MD, MS; Brittany Weber, MD, PhD |
| 12:00pm | BREAK/LUNCH |
Session 3: Constrictive Pericarditis: The Modern Approach | |
| 12:45 | Case Presentation | Fellow |
| 12:50 | Pathophysiology and Hemodynamics of Constrictive Pericarditis | Leonard Lilly, MD |
| 1:10 | Echocardiographic Assessment of Constrictive Pericarditis | Michael Picard, MD |
| 1:30 | Diagnostic Challenges in Radiation-Induced Pericardial Disease | Tom Neilan, MD, MPH |
| 1:45 | Surgical Treatment of Constrictive Pericarditis: What Every Clinician Should Know | Thor Sundt, MD and Shana Osho, MD, MPH |
| 2:15 | Q&A | Leonard Lilly, MD; Michael Picard, MD; Thor Sundt, MD; Shana Osho, MD, MPH |
| 2:30 | BREAK |
| 2:40 | Constrictive Pericarditis: The Patient Perspective | George Blees & Jonathan Salik, MD, MS |
| 2:50 | Complex Case Round Table | Leonard Lilly, MD; Thor Sundt, MD; Shana Osho, MD, MPH |
| 3:10 | Wrap-Up/Final Remarks | Jonathan Salik, MD, MS |
| 3:15pm | Adjourn |
[format] => full_html ) [field_registration_instructions] => Array ( [value] =>
| Registration Type | Early Bird Rate (Before January 15, 2024) | Standard Rate (After January 15, 2024) |
|---|---|---|
| Physicians & Nurses | $150.00 | $199.00 |
| Fellows/Trainees | $50.00 | $50.00 |
Cancellation Policy:
Registrations cancelled on or before February 22, 2024 will be refunded, less a $15 administrative fee. Registrations cancelled after February 22, 2024 will not be refunded.
Contact partnerscpd@partners.org if you require assistance in cancelling your online registration.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for Physicians, Nurses, Physician Assistants in the following specialties Cardiology, Critical Care, Emergency Medicine, General Practice, Geriatric Medicine, Hematology/Oncology, Internal Medicine, Interventional Cardiology, Obstetrics/Gynecology, Peripheral Vascular Disease, Primary Care, Pulmonary Disease, and Sports Medicine.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/2804 [id] => 2804 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital - Corrigan Minehan Heart Center and
Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=70769
[first] => https://cpd.partners.org/node?nid=70769&page=0
[last] => https://cpd.partners.org/node?nid=70769&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Mass General Brigham designates this live activity for a maximum of 7.00 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1714577340
[value2] => 1727063940
[duration] => 12486600
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1720873800
[value2] => 1720904400
[duration] => 30600
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/67479
[id] => 67479
[resource] => file
[uuid] => cffcce83-f0e6-4f9c-adc7-52336deadf0c
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 51571
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Simches Research Center
[street] => 185 Cambridge Street
[additional] =>
[city] => Boston
[province] => MA
[postal_code] => 02114
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => This is an in-person activity.
The Optical Imaging in Neurosurgery Meeting is a gathering of optical imaging experts and neurosurgeons who share a common goal of improving visualization in surgery. This event aims to function both as a showcase of cutting-edge optical imaging technologies and a forum for addressing unmet clinical needs that could potentially be solved by optics-based methods. Through presentation and organized discussion, this meeting seeks to bridge the gap between technological advancement and clinical requirements.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Conference Organizers
Danielle Harper, PhD - Course Co-Director
Instructor, Wellman Center for Photomedicine at Massachusetts General Hospital
Pablo Valdes, MD, PhD - Course Co-Director
Assistant Professor, Department of Neurosurgery, University of Texas Medical Branch
Brett Bouma, PhD
Wellman Center for Photomedicine at Massachusetts General Hospital
Alexandra Golby, MD
Brigham and Women's Hospital
Michael Mooney, MD
Brigham and Women's Hospital
Maxina Sheft
Wellman Center for Photomedicine at Massachusetts General Hospital
Benjamin Vakoc, PhD
Wellman Center for Photomedicine at Massachusetts General Hospital
Martin Villiger, PhD
Wellman Center for Photomedicine at Massachusetts General Hospital
Faculty
Daniel Côté, PhD
Professor, CERVO Brain Research Center
Emily Gibson, PhD
Associate Professor, University of Colorado - Denver
Sylvain Gioux, PhD
Director of Imaging Research, Intuitive Surgical
Costas Hadjipanayis MD, PhD
Executive Vice Chair, Neurological Surgery, University of Pittsburgh
Kevin Huang, MD
Neurosurgeon, Department of Neurosurgery, Brigham & Women's Hospital
Assistant Professor of Neurosurgery, Harvard Medical School
Peter Kan, MD, MPH
Professor, Department of Neurosurgery, University of Texas Medical Branch
Anand Kumar, PhD
Director, Mike Toth Head and Neck Cancer Research Center, Mass Eye and Ear
Frédéric Leblond, PhD
Professor, Department of Engineering Physics, Polytechnique Montreal
John YK Lee, MD
Professor, Department of Neurosurgery, University of Pennsylvania
Anita Mahadevan-Jansen, PhD
Professor, Biophotonics Center, Vanderbilt University
Laura Marcu, PhD
Professor, Department of Biomedical Engineering, UC Davis
Michael Mooney, MD
Neurosurgeon, Department of Neurosurgery, Brigham & Women's Hospital
Assistant Professor of Neurosurgery, Harvard Medical School
Brian Pogue, PhD
Department Chair, Department of Medical Physics, University of Wisconsin Madison
John Rolston, MD, PhD
Neurosurgeon, Department of Neurosurgery, Brigham & Women's Hospital
Associate Professor of Neurosurgery, Harvard Medical School
Timothy Smith, MD, PhD, MPH
Neurosurgeon, Department of Neurosurgery, Brigham & Women's Hospital
Associate Professor of Neurosurgery, Harvard Medical School
Bryan Spring, PhD
Associate Professor, Department of Physics, Northeastern University
Shriya Srinivasan, PhD
Assistant Professor, School of Engineering and Applied Sciences, Harvard University
Eric Suero-Molina, Priv.-Doz. Dr. med
Senior Physician, Department of Neurosurgery, Münster University Hospital
Martin Villiger, PhD
Assistant Professor, Wellman Center for Photomedicine at Massachusetts General Hospital
Lei Wang, PhD
Assistant Professor, School of Medicine, Oregon Health & Science University
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Describe the latest advances in optical imaging that are suitable for neurosurgical applications.
- Identify current unmet needs in neurosurgical visualization.
- Recognize challenges associated with clinical translation of optical tools in neurosurgery.
[format] => full_html
)
[field_program] => Array
(
[value] => 8:30 AM | Welcome Address |
| 8:40 | Session 1: Finding the Tumor |
9:55 | Break |
10:05 | Session 2: Sparing Normal Structures |
| 11:20 | Break |
11:30 | Session 3: Unmet Needs Michael Mooney, MD, Timothy Smith, MD, PhD, MPH, Peter Kan, MD, MPH, John Rolston, MD, PhD & Kevin Huang, MD |
12:45 PM | Lunch & Networking |
| 1:45 | Session 4: Upcoming Technologies Emily Gibson, PhD, Daniel Côté, PhD, Martin Villiger, PhD, Pablo Valdes, MD, PhD, Laura Marcu, PhD, Eric Suero-Molina, Priv.-Doz, Dr.med & Shriya Srinivasan, PhD |
| 3:30 | Transition to Breakout Rooms |
3:35 | Breakout Sessions The Future of Tumor Identification The Future of Sparing Normal Structures How to Integrate Optical Technologies into the Surgical Workflow Unmet Needs |
4:50 | Closing Remarks |
| 4:55 PM | Adjournment |
Networking at the Paul S. Russell, MD Museum of Medical History & Innovation, beginning at 5:00 PM ET. Appetizers & drinks will be available.
[format] => full_html ) [field_registration_instructions] => Array ( [value] =>We can assist you with any special needs (i.e., physical, dietary, parking, etc). Please contact Danielle Harper prior to the live event at djharper@mgh.harvard.edu to make arrangements.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for neurosurgeons, optical imaging specialists and engineers.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3204 [id] => 3204 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>MGH Wellman Center for Photomedicine, Center for Biomedical OCT Research & Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=55418
[first] => https://cpd.partners.org/node?nid=55418&page=0
[last] => https://cpd.partners.org/node?nid=55418&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this live activity for a maximum of 10.25 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 10.25 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity
[summary] =>
[format] => full_html
)
[field_course_catalog] => 1
[field_course_category] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/231
[id] => 231
[resource] => taxonomy_term
[uuid] => 541dec03-c6af-4bcb-9af7-8fa28fedfb53
)
[1] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/232
[id] => 232
[resource] => taxonomy_term
)
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1672852860
[value2] => 1686628740
[duration] => 13775880
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1683028800
[value2] => 1683046800
[duration] => 18000
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
[0] => Array
(
[uri] => https://cpd.partners.org/taxonomy_term/238
[id] => 238
[resource] => taxonomy_term
[uuid] => fd81c17a-d19b-46b8-ad6b-2c5aee9ce9be
)
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/42893
[id] => 42893
[resource] => file
[uuid] => fc651756-f3ee-4beb-b956-f1d28519753a
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
[lid] => 34187
[latitude] => 0.000000
[longitude] => 0.000000
[name] => Westin Copley Place
[street] => 10 Huntington Avenue
[additional] =>
[city] => Boston
[province] => MA
[postal_code] => 02116
[country] => us
[province_name] => Massachusetts
[country_name] => United States
[phone] =>
[fax] =>
[email] =>
[www] =>
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => This is a Hybrid Event. Registrants will be able to choose if they would like to attend in-person or virtually.
Cancer treatment has evolved significantly over the past decade from a treatment paradigm anchored on surgery, chemotherapy, and radiotherapy, to one embracing molecularly-targeted therapies disrupting tumor-specific signaling pathways, as well as new approaches to mobilize the immune system. For clinicians trying to keep current with advancing immuno-oncology principles and research, the pace of these developments has brought new challenges. Recognizing these challenges, this course will provide a comprehensive clinical review of the advances taking place in the immuno-oncology field.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] => Course Directors
Justin Gainor, MD
Director, Center for Thoracic Cancers,
Director of Targeted Immunotherapy,
Massachusetts General Hospital Cancer Center;
Associate Professor of Medicine, Harvard Medical School
Krista Rubin, MS, FNP-BC
Nurse Practitioner, Center for Melanoma,
Massachusetts General Hospital Cancer Center
Ryan Sullivan, MD
Physician Investigator, Cancer Center, Mass General Research Institute;
Assistant In Medicine, Hematology-Oncology, Massachusetts General Hospital;
Associate Professor of Medicine, Harvard Medical School
Faculty
Jeremy Abramson, MD
Director, Jon and Jo Ann Hagler Center for Lymphoma,
Massachusetts General Hospital Cancer Center;
Associate Professor of Medicine, Harvard Medical School
Hugh Auchincloss, MD
Thoracic Surgery,
Massachusetts General Hospital
Mark Awad, MD, PhD
Clinical Director, Thoracic Oncology Treatment Center,
Dana-Farber Cancer Institute;
Associate Professor of Medicine, Harvard Medical School
Steven Blum, MD
Instructor in Medicine,
Massachusetts General Hospital
Genevieve Boland, MD, PhD
Vice Chair of Research, Department of Surgery,
Director, Therapeutic Intralesional Program,
Surgical Director, Termeer Center for Targeted Therapies,
Massachusetts General Hospital
Jonathan H. Chen, MD, PhD
Instructor in Pathology,
Massachusetts General Hospital
Riley Fadden, MSN, RN, FNP-C
Nurse Practitioner, Center for Melanoma,
Massachusetts General Hospital Cancer Center
Florian Fintelmann, MD
Radiologist, Thoracic Imaging and Intervention,
Head, Thoracic Imaging Percutaneous Thermal Ablation,
Massachusetts General Hospital;
Associate Professor, Harvard Medical School
Ruth Foreman, MD
Assistant Pathologist, Dermatopathology Service,
Massachusetts General Hospital;
Instructor, Harvard Medical School
Xin Gao, MD
Assistant in Medicine,
Massachusetts General Hospital Cancer Center;
Assistant Professor, Harvard Medical School
Rakesh Jain, PhD
Director, Steele Laboratory, Massachusetts General Hospital;
A. Werk Cook Professor of Radiation Oncology, Harvard Medical School
Howard Kaufman, MD
Assistant in Surgery, Surgery, Massachusetts General Hospital;
Lecturer in Surgery, Harvard Medical School
Florence (Katie) Keane, MD
Assistant Professor in Radiation Oncology,
Massachusetts General Hospital
Jason J. Luke, MD, FACP
Director of the Cancer Immunotherapeutics Center,
University of Pittsburgh
Mari Mino-Kenudson, MD
Director, Pulmonary Pathology,
Pathologist, Massachusetts General Hospital;
Professor of Pathology, Harvard Medical School
Patrick Ott, MD, PhD
Clinical Director, Melanoma Disease Center,
Director, Clinical Sciences, Center for Immuno-Oncology,
Dana-Farber Cancer Institute;
Associate Professor of Medicine, Harvard Medical School
Jong Chul Park, MD
Assistant Professor of Medicine,
Massachusetts General Hospital Cancer Center
Laura Petrillo, MD
Palliative Care Physician, Massachusetts General Hospital;
Assistant Professor of Medicine, Harvard Medical School
Arlene Sharpe, MD, PhD
Kolokotrones University Professor,
Chair, Department of Immunology,
Harvard Medical School
Alexandra-Chloe Villani, PhD
Director, Single-Cell Genomics Program,
Center for Immunology and Inflammatory Diseases,
Massachusetts General Hospital;
Assistant Professor of Medicine, Harvard Medical School;
Associate Scientist, Broad Institute of MIT and Harvard
Leyre Zubiri, MD, PhD
Immunotherapy Toxicity Fellow,
Severe Immunotherapy Complications Service,
Massachusetts General Hospital Cancer Center
[format] => full_html
)
[field_hardware_software] => Array
(
)
[field_hotel_information] => Array
(
[value] => Accommodations:
A limited number of rooms have been reserved at The Westin Copley Place for the nights of April 30 and May 1 at nightly rate of $279. Hotel room rates are subject to applicable state and local taxes in effect at the time of check-out. To book your room, contact the hotel at (617) 262-9600 or CLICK HERE to reserve online. The reservation deadline is Friday, April 7, 2023.
[format] => full_html
)
[field_hotel_link] => Array
(
)
[field_hotel_photo] => Array
(
)
[field_hotel_travel] => Array
(
)
[field_learning_objectives] => Array
(
[value] => Upon completion of this activity, participants will be able to:
- Evaluate cancer immunotherapy principles and strategies and how they influence current treatment approaches.
- Identify the emerging role of personalized cancer vaccination and other immunotherapy combinations in patients with solid tumor and hematologic malignancies.
- Define currently approved and emerging predictive biomarkers for cancer immunotherapy.
- Recognize and implement management strategies for immune-mediated side effects in patients treated with immunotherapy agents.
- Recognize the importance of establishing a multidisciplinary approach in the immunotherapy era.
For exhibit space, please contact ebrooks3@mgh.harvard.edu
[format] => full_html
)
[field_program] => Array
(
[value] => Monday, May 1, 2023 | 7:30am - 4:15pm
7:30 am | Registration and Breakfast |
8:00 | Welcome | Justin Gainor, MD; Krista Rubin, MS, FNP-BC; Ryan Sullivan, MD |
8:05 | Primer | Howard L. Kaufman, MD |
8:35 | Q&A |
8:45 | Overview of Immunology Tolerance | Arlene Sharpe, MD, PhD |
9:15 | Q&A |
9:25 | Cancer Immunotherapy: Where are We Now? | Justin Gainor, MD |
9:55 | Q&A |
| 10:05 | BREAK |
10:20 | Cellular Therapies Lecture | Jeremy Abramson, MD |
10:50 | Q&A |
11:00 | Normalizing the Tumor Microenvironment to Improve Cancer Immunotherapy: Bench to Bedside | Rakesh Jain, PhD |
11:30 | Q&A |
| 11:40 | RAPID FIRE!!! Cancer Immunotherapy for the Non-Medical Oncologist Panelists:
|
12:25pm | LUNCH |
1:25 | Palliative Care | Laura Petrillo, MD |
1:50 | Q&A |
2:00 | Mechanisms of Immunotherapy Toxicity | Alexandra-Chloe Villani, PhD |
2:30 | Q&A |
2:40 | BREAK |
2:50 | Toxicity – Clinical (and Practical) | Krista Rubin, MS, FNP-BC and Riley Fadden, MSN, RN, FNP-C |
3:15 | Q&A |
3:25 | Interactive Case Studies | Steve Blum, MD & Leyre Zubiri, MD, PhD |
4:10 | Closing Remarks |
| 4:15 pm | Adjourn |
Tuesday, May 2, 2023 | 7:30am - 1:00pm
7:30 am | Registration and Breakfast |
8:00 | Welcome | Justin Gainor, MD; Krista Rubin, MS, FNP-BC; Ryan Sullivan, MD |
8:05 | Resistance Biomarkers | Jonathan Chen, MD, PhD |
| 8:35 | Q&A |
8:45 | Biomarkers Debate: Pragmatic vs. Perfect | |
9:15 | Q&A |
9:25 | Incorporating Biomarker Analysis into Optimal Treatment Selection | |
9:55 | Q&A |
| 10:05 | BREAK |
10:25 | Navigating Clinical Trial Data to Help Make Right Choice for Your Patient | |
| 10:55 | Q&A |
11:05 | Incorporating Checkpoint Inhibitors into Multidisciplinary Care | Hugh Auchincloss, MD; Genevieve Boland, MD, PhD; Justin Gainor, MD; Katie Keane, MD; Jason Luke, MD, FACP; Mari Mino-Kenudson, MD |
11:35 | Q&A |
11:45 | RAPID FIRE!!! What’s Next in Immunotherapy?
|
12:15 pm | Q&A |
12:25 | Wrap-Up Session | Justin Gainor, MD; Krista Rubin, MS, FNP-BC; Ryan Sullivan, MD
|
12:55 pm | Adjourn |
[format] => full_html ) [field_registration_instructions] => Array ( [value] =>
| Registration Type | Tuition Fee |
|---|---|
| Physician: In-Person | $159.00 |
| Physician: Virtual | $89.00 |
| Fellows/Nurses/PAs/etc.: In-Person | $109.00 |
| Fellows/Nurses/PAs/etc.: Virtual | $39.00 |
| Industry: In-Person | $399.00 |
| Industry: Virtual | $299.00 |
Cancellation Policy:
Registrations cancelled on or before April 17, 2023 will be refunded, less a $25 administrative fee. Registrations cancelled after April 17, 2023 will not be refunded.
Contact partnerscpd@partners.org if you require assistance in cancelling your online registration.
Accommodations:
A limited number of rooms have been reserved at The Westin Copley Place for the nights of April 30 and May 1 at nightly rate of $279. Hotel room rates are subject to applicable state and local taxes in effect at the time of check-out. To book your room, contact the hotel at (617) 262-9600. The reservation deadline is Friday, April 7, 2023.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for physicians, nurses, physician assistants, and other members of the healthcare team.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/2500 [id] => 2500 [resource] => accme_data ) [field_show_on_calendar] => 1 [field_custom_provided] => Array ( [value] =>Massachusetts General Hospital Cancer Center & Mass General Brigham
Array
(
[self] => https://cpd.partners.org/node?nid=82905
[first] => https://cpd.partners.org/node?nid=82905&page=0
[last] => https://cpd.partners.org/node?nid=82905&page=0
[list] => Array
(
[0] => Array
(
[field_course_rating_access] => none
[uc_product_image] => Array
(
)
[field_accreditation] => Array
(
[value] => In support of improving patient care, Mass General Brigham is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Credit Designation Statements
AMA PRA Category 1 CreditsTM
Mass General Brigham designates this live activity for a maximum of 3.25 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing
Mass General Brigham designates this activity for 3.25 ANCC contact hours. Nurses should only claim credit commensurate with the extent of their participation in the activity.
Social Work
As a Jointly Accredited Organization, Mass General Brigham is approved to offer social work continuing education by the Association of Social Work Boards (ASWB) Approved Continuing Education (ACE) program. Organizations, not individual courses, are approved under this program. State and provincial regulatory boards have the final authority to determine whether an individual course may be accepted for continuing education credit. Mass General Brigham maintains responsibility for this course. Social workers completing this course receive 3.25 continuing education credit.
Lifelong Learning Maintenance of Certification (MOC) Program
American Board of Internal Medicine's (ABIM)
MOC COMPLETION CRITERIA
Participant completion for MOC points will be reported to the boards when credit is awarded for the session.
MOC points can only be awarded if you attended the entire session.
Lifelong Learning MOC points in the American Board of Internal Medicine's (ABIM) Maintenance of Certification (MOC) Program
Upon successful completion of this activity, if you wish to receive MOC Part 2 points you will need to enter your ABIM ID number and birthday (month/day) in your profile. The Mass General Brigham Office of Continuing Professional Development will verify completion of the activity and report to the ABIM. . Diplomates are responsible for checking their ABIM Portfolio for confirmation of MOC Part 2 points.
MOC RECOGNITION STATEMENT
Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to 3.25 MOC points in the American Board of Internal Medicine’s (ABIM) Maintenance of Certification (MOC) program. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
[summary] =>
[format] => full_html
)
[field_course_catalog] =>
[field_course_category] => Array
(
)
[field_course_completion_message] => Array
(
)
[field_course_date] => Array
(
[value] => 1736521680
[value2] => 1746071940
[duration] => 9550260
)
[field_course_disclosure] => Array
(
)
[field_course_event_date] => Array
(
[value] => 1744380000
[value2] => 1744392600
[duration] => 12600
)
[field_course_external_url] => Array
(
)
[field_course_format] => Array
(
)
[field_course_image] => Array
(
[file] => Array
(
[uri] => https://cpd.partners.org/file/80725
[id] => 80725
[resource] => file
[uuid] => e897be3b-dc3a-411f-a26b-72fe3b277d02
)
)
[field_course_intro] => Array
(
)
[field_course_live] => 1
[field_course_location] => Array
(
)
[field_course_password] =>
[field_course_rating] => Array
(
)
[field_course_restrict_role] => Array
(
)
[field_course_summary] => Array
(
[value] => This is a virtual course
The second Community Care in Reach® (CCiR) Mobilizing Addiction Services conference will highlight strategies & best practices around mobilizing clinical care and harm reduction services for people living with addiction. Subject matter experts from across the country will present their expertise & knowledge on topics spanning several aspects of mobile and addiction care, including safety & de-escalation in a mobile setting, the role of mobile programs in combatting stigma around addiction, and how to navigate providing addiction care in our evolving political and social landscape.
[summary] =>
[format] => full_html
)
[field_course_transcript] => 1
[field_enrollment_requirement_min] =>
[field_enrollment_requirements] => Array
(
)
[field_faculty_credentials] => Array
(
[value] =>  | Elsie Taveras, MD, MPH - Course Director Chief Community Health & Equity Officer, Mass General Brigham Executive Director, Kraft Center for Community Health at Massachusetts General Hospital Conrad Taff Professor of Pediatrics in Nutrition, Harvard Medical School Professor in the Department of Nutrition, Harvard T.H. Chan School of Public Health |
 | Erik Garcia, MD Erik Garcia, MD has been been providing healthcare to adults experiencing homelessness for the entirety of his career – starting when he completed his Internal Medicine residency in 1994. He is married to a doctor (the research, PhD kind…"smarter than me" he says) who is incredibly supportive. They have 2 grown kids who (while they have avoided the medical field) have a wonderful sense of social consciousness. |
 | Sarah Mackin, MPH Sarah Mackin, MPH is the director of AHOPE Needle Exchange at the Boston Public Health Commission, where she began her work in harm reduction and drug user health in 2010. She oversees the largest needle exchange and harm reduction program in New England, which provides comprehensive drug user health services to over 8,000 people each year. Sarah brings over 18 years of experience in the field of public health, substance use, harm reduction, HIV/AIDS, and homelessness to the work. |
 | Maritza Perez Medina, JD Maritza Perez Medina manages DPA's federal legislative agenda and advocacy strategy in Congress as well as DPA’s general engagement with the federal government on its policy priorities. Previously, Maritza was a Senior Policy Analyst for Criminal Justice Reform at the Center for American Progress (CAP). Prior to joining CAP, Maritza was a Legislative Staff Attorney at the Mexican American Legal Defense and Educational Fund (MALDEF) where she advocated on a range of civil rights issues impacting Latino communities. Originally from Nevada, Maritza obtained her B.A. from the University of Nevada, Reno with academic honors, graduating with double majors in journalism and Spanish and double minors in political science and economic policy. She earned her J.D. at the University of California, Berkeley, School of Law, receiving the highest distinction upon graduation for her pro bono work, and is licensed to practice law in the District of Columbia and in the state of California. A criminal justice and drug policy expert, Maritza has been featured in various media outlets including The Washington Post, The New York Times, Los Angeles Times, The Wall Street Journal, Politico, Roll Call, The Boston Globe, CNN, USA Today, Chicago Tribune, NPR, Latino USA, and more. |
 | Kenneth Washington Kenneth Washington is an accomplished assistant director of AHOPE Needle Exchange, driven by a passion for harm reduction that stems from his work with at-risk youth. His lived experience has instilled in him a deep understanding of the challenges of racism, classism, and substance use, inspiring him to become a leader in the field. Kenneth's outstanding achievements in harm reduction have earned him a seat on the Massachusetts Harm Reduction Advisory Council, a testament to his unwavering dedication to public service. His desire to help his community has led him to excel in drug checking and introduce innovative safer smoking practices to the Boston area outreach. With his profound knowledge and expertise, Kenneth has made a significant impact on the lives of countless individuals and helped to shape policies that promote safer and healthier communities. His contributions have been widely recognized and admired by peers, colleagues, and stakeholders alike. |
[format] => full_html ) [field_hardware_software] => Array ( ) [field_hotel_information] => Array ( ) [field_hotel_link] => Array ( ) [field_hotel_photo] => Array ( ) [field_hotel_travel] => Array ( ) [field_learning_objectives] => Array ( [value] =>
Upon completion of this activity, participants will be able to:
- Describe the CCiR mobile addiction services model that uses cross-sector collaborations to reduce siloing of services, especially between harm reduction and clinical care.
- Apply safety and de-escalation strategies for teams on mobile units.
- Apply effective strategies for destigmatizing addiction care in mobile settings.
- Assess elements of effective outreach and engagement.
- Design an effective community engagement strategy in advance of mobile program launch.
- Describe local, regional, and national trends, events, and contexts that may impact a mobile team’s ability to provide effective addiction and harm reduction services.
- Use strategies to effectively provide and advocate for mobile addiction care considering new developments in the legal, political, and social landscape.
| 10:00 AM | Introduction | Elsie Taveras, MD, MPH |
| 10:15 | Combating Addiction Stigma: What Role Can Mobile Programs Play? | Erik Garcia, MD |
| 11:20 | De-Escalation & Staying Safe in Close Quarters | Sarah Mackin, MPH & Kenneth Washington |
| 12:20 PM | Break |
| 12:35 | Changing Political Climate: Tools & Resources | Maritza Perez Medina, JD |
| 1:25 | Closing Remarks | Jen Tracey |
| 1:30 PM | Adjournment |
[format] => full_html ) [field_registration_instructions] => Array ( [value] =>
A recording of the conference is now available in the course outline. To access it, please click the blue 'Take Course' button.
[summary] => [format] => full_html ) [field_related_courses] => Array ( ) [field_requirements_max] => [field_requirements_min] => [field_show_child_catalog] => [field_show_child_transcript] => [field_target_audience] => Array ( [value] =>This activity is intended for physicians, nurses, social workers and other members of the healthcare team with specialties of addiction medicine & primary care.
[format] => full_html ) [field_venue_phone] => Array ( ) [upload] => Array ( ) [field_accme_data] => Array ( [uri] => https://cpd.partners.org/accme_data/3663 [id] => 3663 [resource] => accme_data ) [field_show_on_calendar] => [field_custom_provided] => Array ( [value] =>Kraft Center for Community Health, Massachusetts General Brigham Center for Community Health, RIZE Massachusetts & Mass General Brigham